Headache / Migraine
Headache and Migraine: Understanding Pain, Diagnosis, and Relief
Many people experience headaches as part of their daily life, but when pain becomes severe, frequent, or debilitating, it deserves proper attention and care. This page explains the difference between everyday headaches and migraines, why they happen, how they are diagnosed, and what treatments are available. It is for education only and does not replace advice from your own doctor.
What Is the Difference Between a Headache and a Migraine?
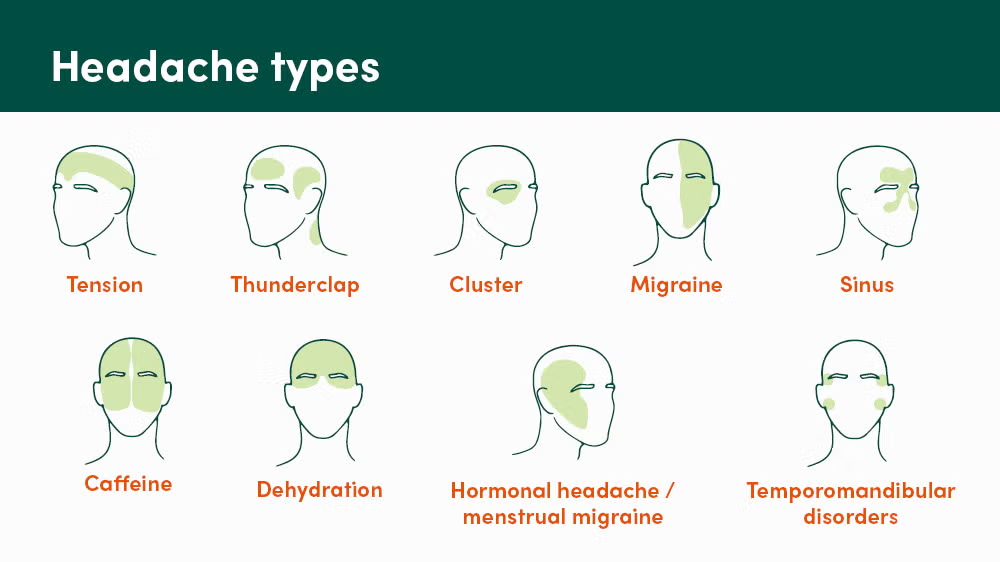
A headache is any form of pain or discomfort in the head, scalp, or neck area. It is very common and usually mild to moderate. A migraine, on the other hand, is a complex neurological condition that goes far beyond just head pain. While all migraines are a type of headache, not all headaches are migraines.
The differences matter because they affect how you feel and what treatment will help. A tension headache typically feels like a dull, tight, pressure-like sensation that may last from 30 minutes to a few hours and often affects both sides of the head. It is usually manageable with rest and over-the-counter pain relievers.
A migraine, however, is typically a throbbing or pulsating pain that usually affects one side of the head. It can last 4 to 72 hours and is often so severe that it interferes with daily activities. Migraines are usually accompanied by other symptoms such as nausea, vomiting, sensitivity to light and sound, and sometimes visual disturbances.
Why Do Migraines Happen?
The exact cause of migraines is not completely understood, but researchers believe migraines occur because something abnormal happens in the brain that disrupts nerves, chemicals, and blood vessels. Both genetic and environmental factors play an important role.
If your parents or siblings have migraines, you are more likely to have them too. This is because migraines tend to run in families. Beyond genetics, many other things can influence whether you have a migraine. These include stress, hormonal changes (especially in women), lack of sleep, skipping meals, dehydration, certain foods and drinks, bright or flashing lights, strong smells, and weather changes.
Common migraine triggers include stress, certain foods like red wine and processed meats, caffeine, chocolate, aged cheeses, and foods containing MSG. Caffeine withdrawal can also be a trigger, which is why suddenly stopping coffee or tea may cause a migraine. For women, hormonal changes related to the menstrual cycle, pregnancy, or birth control pills can trigger migraines.
It is important to understand that triggers do not cause migraines in the same way a light switch works. Instead, think of it as a threshold. When enough triggers pile up at the same time, you are more likely to have a migraine. For example, missing lunch alone might be fine one day, but missing lunch while also being sleep-deprived and stressed might be enough to trigger an attack.
Recognizing Migraine Symptoms
Migraines often develop in stages, and understanding these stages helps you manage them better. Many people experience warning signs 1 to 2 days before a migraine starts. These early signs might include mood changes, fatigue, food cravings, or neck stiffness. This early phase is called the prodrome.
Some people then experience an aura, which happens before the actual headache pain begins. An aura involves temporary visual disturbances, numbness, tingling, or difficulty speaking. Not everyone with migraines has an aura, but those who do usually experience it for 20 to 60 minutes before the headache begins. You might see flashing lights, zigzag patterns, or blind spots. Some people feel numbness on one side of the body or have difficulty finding words.
The actual migraine attack is when the intense head pain begins. The pain is typically one-sided and pulsating or throbbing in nature, though it can spread to other areas. Along with the pain, you may experience nausea, vomiting, extreme sensitivity to light (photophobia), sensitivity to sound (phonophobia), sensitivity to smell, and sometimes watery eyes or a runny nose. Many people feel relief in dark, quiet rooms and may sleep to escape the pain.
After the migraine ends, you may experience what is called a postdrome phase. During this time, you might feel brain fog, fatigue, weakness, or lingering tiredness that can last several hours to a day. Some people feel energised after a migraine ends, while others feel completely exhausted.
How Are Migraines and Headaches Diagnosed?
Proper diagnosis is essential because headaches and migraines can sometimes indicate other medical conditions that need attention. Your doctor can diagnose migraine by asking about your symptoms and family history. They will perform a complete physical and neurological exam to determine if your headaches are due to muscle tension, sinus problems, or a different condition.
During the evaluation, your doctor will ask detailed questions about your headaches: When did they start? How often do they occur? How long do they last? What does the pain feel like? Where is the pain located? What makes it better or worse? Do you have any warning signs before they start? What other symptoms occur with the headache?
It is very helpful to keep a headache diary before seeing your doctor. Write down when headaches occur, what you were doing before they started, what you ate, how much you slept, stress levels, and any other symptoms. This information helps your doctor identify patterns and triggers.
In most cases, no special tests are needed to diagnose migraines. There is no specific blood test or scan that proves you have a migraine. However, your doctor may order a brain CT or MRI scan if you have certain neurologic symptoms, such as weakness, memory problems, or loss of alertness, especially if this is a new type of headache for you.
When and Why Medical Evaluation Is Important
Not every headache requires a doctor’s visit, but certain situations demand prompt medical attention. If your headaches are increasing in frequency or severity, or are interfering with your daily activities, you should see a doctor.
Seek immediate medical attention if your headache comes on suddenly and becomes severe very quickly, feels like the worst headache you have ever experienced, is accompanied by a stiff neck and fever, involves seizures, fainting, confusion or personality changes, begins right after an injury or head trauma, is accompanied by weakness, numbness or vision changes, or lasts more than 72 hours.
Medical evaluation is important because persistent headaches can sometimes indicate other medical conditions that need treatment. Early consultation helps identify any underlying problems and starts appropriate management before headaches become more frequent or severe.
How Migraines and Headaches Are Treated
Treatment depends on the type of pain you are experiencing and how often it occurs. For tension headaches, over-the-counter pain relievers like paracetamol or ibuprofen usually work well. Relaxation techniques, heat therapy, and neck massage can also help.
Migraine treatment is different and works in two ways. Pain-relieving medicines, also called acute or abortive treatments, are taken during migraine attacks to stop symptoms. These work best when taken early in the attack, before the pain becomes severe. Common options include triptans, ergotamines, and pain relievers combined with other medications.
Preventive medicines are taken regularly, often daily, to reduce how often migraines occur and how severe they are. These include certain blood pressure medicines, antidepressants, anti-seizure medications, and newer medications specifically designed for migraine prevention. Your doctor chooses preventive treatment based on how often you have migraines, how disabling they are, and any other health conditions you have.
Antinausea medicines are usually taken with pain medicines and help if you experience nausea and vomiting with your migraines. Your doctor may also recommend non-medication options such as biofeedback, relaxation techniques, cognitive behavioral therapy, and special devices designed to treat migraine pain.
Beyond medications, stress management through relaxation therapy, meditation, and exercise can be extremely helpful in managing and preventing migraines. Maintaining a consistent sleep schedule, staying hydrated, eating regular meals, and avoiding known triggers all play important roles in reducing migraine frequency and severity.
Managing Triggers and Prevention
One of the best things you can do is learn your personal migraine triggers that cause pain or other migraine symptoms. Everyone’s triggers are different, so what triggers a migraine for one person may not affect another. The first step is to track your migraine symptoms in a notebook, diary, or smartphone app.
Note what you were doing before and when your migraine symptoms began. What had you eaten? Were you dehydrated? How much sleep did you get the night before? Did anything stressful or exciting happen that day? Over time, patterns will emerge showing your personal triggers.
Common triggers include stress, irregular or poor sleep, hormonal changes, skipped meals, caffeine, alcohol, dehydration, bright lights, strong smells, and weather changes. Some people also react to certain foods or food additives.
Once you identify your triggers, you can work to manage them. Staying well hydrated by carrying a water bottle and drinking enough fluids every day can prevent dehydration-related migraines. Try to go to bed at the same time every night and aim to get at least 7-8 hours of sleep, which is one of the most important migraine prevention strategies.
Making a list of things that cause you stress and working to reduce these triggers in your life helps significantly. Biofeedback, relaxation therapy, meditation, and exercise can change your body’s response to stress and reduce migraines. While you cannot eliminate all stress, these strategies make your brain less reactive to it.
Why You Should See a Neurologist for Migraines
A neurologist is a doctor who specializes in brain and nervous system disorders and is best trained to evaluate and manage migraines. You should see a neurologist if your headaches don’t improve despite taking over-the-counter pain relievers, if headaches are increasing in frequency or severity, if they are interfering with your daily life, or if you need help identifying and managing your triggers.
A neurologist can confirm that what you are experiencing is truly a migraine and not another condition mimicking migraine symptoms. They can prescribe preventive medications if your migraines are frequent, order appropriate tests if needed, and discuss advanced treatment options. They can also guide you on managing work, school, driving, and other activities around your migraine pattern.
If your migraines are frequent and disabling, a neurologist can help reduce the frequency and severity so that you are not having attacks more than twice a week. Even if preventive treatment does not eliminate all migraines, it can significantly improve your quality of life by making attacks less frequent and less severe.
Living Well With Migraines
Many people with migraines learn to manage their condition and live full, productive lives. The key is understanding your personal triggers, taking medications as prescribed, maintaining a consistent lifestyle, and working closely with your healthcare provider.
Creating and following a daily routine helps prevent migraines. This includes maintaining regular sleep and wake times, eating at consistent times, staying hydrated throughout the day, and managing stress effectively. When you do have a migraine attack, knowing your personal pattern helps you respond quickly with appropriate treatment.
It is also important to communicate with your family, friends, and colleagues about your migraines so they understand when you need rest or support. Many employers and schools now provide accommodations for people with migraines.
Frequently Asked Questions About Headaches and Migraines
What is the difference between a headache and a migraine?
A headache is generally mild to moderate pain that lasts 30 minutes to a few hours. A migraine is more severe, usually one-sided, throbbing pain that lasts 4 to 72 hours and is accompanied by symptoms like nausea, vomiting, and sensitivity to light and sound. Migraines often interfere with daily activities while headaches usually do not.
Are migraines hereditary?
Yes, migraines tend to run in families. If your parents or siblings have migraines, you are more likely to have them too. However, having a family history does not mean you will definitely have migraines.
Can certain foods trigger migraines?
Yes, some people find that certain foods trigger migraines. Common culprits include red wine, aged cheeses, processed meats, chocolate, caffeine, and foods containing MSG. However, triggers vary from person to person. Keeping a food diary can help identify which foods, if any, trigger your migraines.
How can I prevent migraines?
Preventing migraines involves identifying and managing your personal triggers. General strategies include maintaining regular sleep and meal times, staying hydrated, managing stress, avoiding known triggers, regular exercise, and taking preventive medications if recommended by your doctor.
Why does my migraine get worse with activity?
Physical activity can intensify migraine pain for many people. This is why people with migraines often seek rest and quiet during an attack. Talk to your doctor about when it is safe to be active and when rest is better.
Can stress cause migraines?
Yes, stress is one of the most common migraine triggers. Both the stress itself and the relaxation period after stress ends can trigger attacks. Managing stress through relaxation techniques, exercise, meditation, and counselling can help reduce migraine frequency.
What should I do during a migraine attack?
Find a dark, quiet place and lie down if possible. Take your prescribed migraine medication as soon as symptoms begin, before the pain becomes severe. Apply heat or cold to your head, neck, or temples. Try relaxation techniques. If symptoms are severe or do not improve, seek medical attention.
Can birth control pills trigger migraines?
For some women, hormonal changes related to birth control can trigger migraines. If you notice your migraines get worse after starting birth control, talk to your doctor. They may adjust your prescription or recommend alternative birth control methods.
When should I see a doctor for a migraine?
See a doctor if migraines are new, increasing in frequency or severity, different from your usual pattern, or if they are interfering with your daily life. Seek immediate medical attention if a migraine feels different than usual, lasts longer than 72 hours, or is accompanied by concerning symptoms like vision loss, weakness, or confusion.
Is there a cure for migraines?
There is currently no cure for migraines, but they can be effectively managed with medication, trigger identification, and lifestyle changes. Many people experience long periods of migraine-free time with proper management.
Can children have migraines?
Yes, children can have migraines, though they may present differently than in adults. Children's migraines may last shorter periods, involve different symptoms, and may be triggered by different things. If you suspect your child has migraines, consult a pediatric neurologist.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you are experiencing persistent, severe, or changing headaches, seek medical advice promptly.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
Last Updated: November 2025
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
