Stroke
Stroke: Understanding Warning Signs, Treatment, and Recovery
A stroke can happen suddenly to anyone, at any time. But the encouraging news is that most stroke survivors recover significantly and regain independence with proper treatment and rehabilitation. When you recognize the warning signs and act quickly, you can minimize damage and set the stage for successful recovery. This page explains what a stroke is, what causes it, how to recognize the warning signs, and what happens during treatment and recovery. It is for education only and does not replace advice from your own doctor.
What Is a Stroke?
A stroke occurs when blood supply to part of the brain is blocked or interrupted, preventing brain tissue from getting oxygen and nutrients. Brain cells begin to die within minutes without oxygen. This medical emergency is also called a brain attack because, like a heart attack, time is critical.
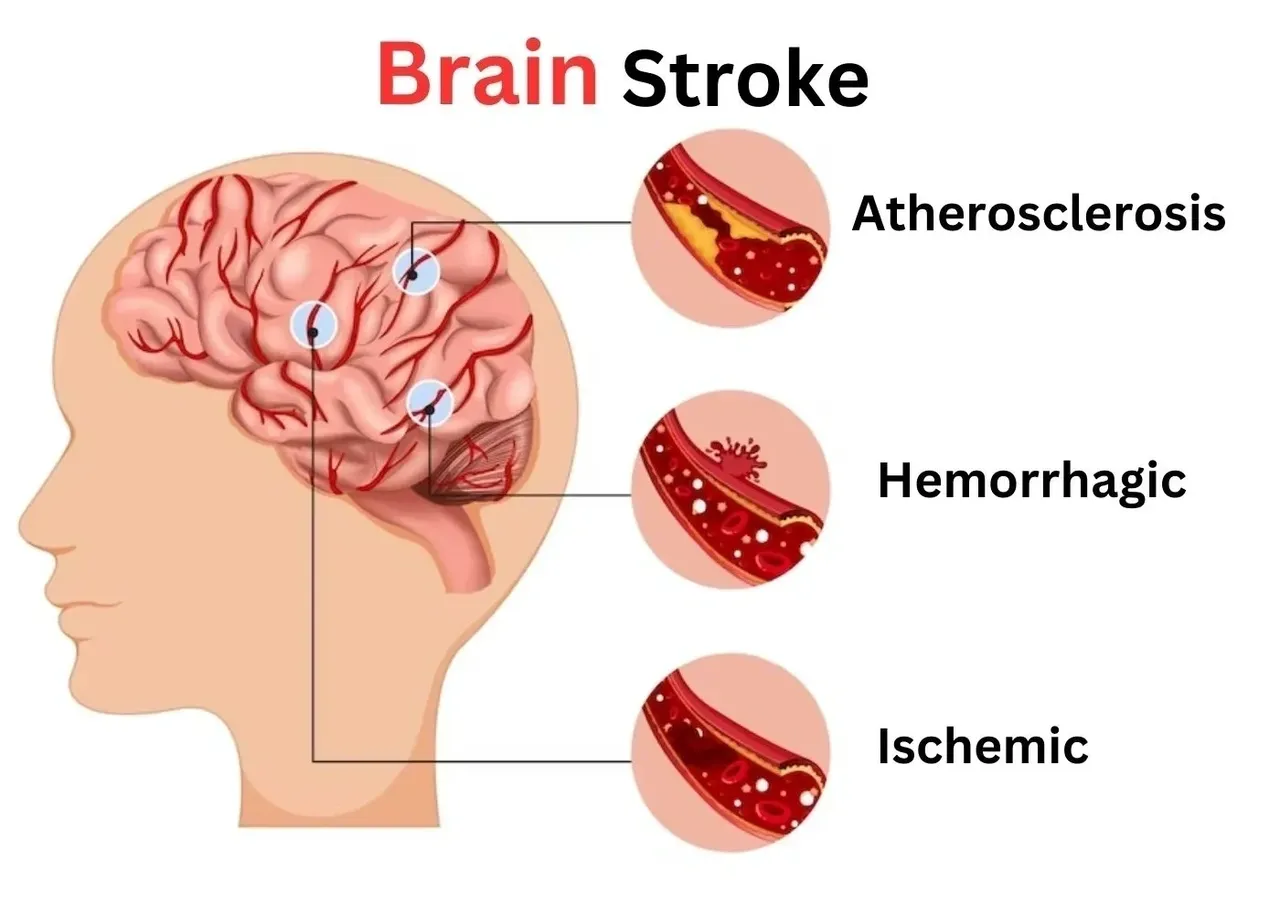
There are two main types of strokes. Ischemic stroke happens when a blood clot or debris blocks a blood vessel in the brain and accounts for approximately 87% of all strokes. This is the most common type and results from fatty deposits that narrow arteries or clots that travel from the heart. Hemorrhagic stroke occurs when a blood vessel in the brain ruptures or leaks, causing bleeding inside the brain. While less common, hemorrhagic strokes are often more severe.
There is also a transient ischemic attack, or TIA, often called a mini-stroke or warning stroke. A TIA causes temporary symptoms that resolve within minutes to hours. Although symptoms disappear, a TIA is a serious warning sign that you are at high risk for a full stroke and requires immediate medical evaluation.
Understanding the Types of Stroke
Ischemic strokes happen in two ways. Thrombotic strokes occur when a blood clot forms directly in an artery leading to the brain, usually in narrowed arteries damaged by fatty buildup. Embolic strokes happen when a blood clot forms elsewhere in the body (often in the heart) and travels through the bloodstream until it lodges in a brain artery, blocking blood flow.
Hemorrhagic strokes result from weakened blood vessels that rupture. High blood pressure is the most common cause, as constant pressure damages blood vessel walls over time. Other causes include brain aneurysms (ballooning in blood vessel walls) and arteriovenous malformations (tangled blood vessels). Approximately 80% of all strokes are preventable through managing risk factors like high blood pressure, diabetes, smoking, and high cholesterol.
Critical Warning Signs: Know F.A.S.T.
The most important thing you can do is recognize stroke symptoms immediately. Time is literally brain—every minute that passes, approximately two million brain cells die. The acronym F.A.S.T. helps you remember the key warning signs of stroke.
F = Face Drooping: Look for one side of the face drooping or feeling numb. Ask the person to smile—if the smile is uneven or lopsided, that is a warning sign. The facial droop happens because stroke affects one side of the brain, which controls the opposite side of the body.
A = Arm Weakness: One arm may feel weak or numb, or drift downward when raised. Ask the person to raise both arms. If one arm cannot stay up or drifts down, that is a stroke warning sign. This weakness often affects only one side of the body.
S = Speech Difficulty: Speech may become slurred, difficult to understand, or the person may be unable to speak. They might also have trouble understanding what you are saying. This happens when the stroke affects the language areas of the brain.
T = Time to Call 911: If you notice any of these three signs, call 911 immediately, even if the symptoms seem mild or if they go away. Record the exact time symptoms started because doctors use this information to decide on treatment. Do not wait. Do not drive to the hospital yourself. Call emergency services so that treatment can begin immediately.
Other Important Stroke Symptoms
Beyond F.A.S.T., other sudden symptoms also indicate stroke. Sudden vision loss or double vision in one or both eyes, sudden severe headache unlike anything experienced before, sudden dizziness or loss of balance and coordination, sudden trouble walking or stumbling, sudden numbness or weakness in the face, arm, or leg (usually on one side), and sudden confusion or difficulty understanding speech.
Any of these symptoms appearing suddenly warrant calling 911 immediately. Some people have silent strokes where symptoms are not obvious but brain cells are still dying. This is why regular medical check-ups and managing risk factors are important.
When Every Minute Counts: Emergency Treatment
When you arrive at the hospital, doctors work with remarkable speed to determine the type of stroke and begin treatment. For ischemic stroke, the goal is to restore blood flow to the brain as quickly as possible. Clot-busting medications called thrombolytics can dissolve blood clots, but must be given within a narrow window, usually within 4.5 hours of symptom onset. The sooner treatment begins, the more brain tissue is saved.
In some cases, mechanical thrombectomy may be performed, where a catheter removes the clot directly from the blocked artery. This procedure can be effective even beyond the standard medication window. For hemorrhagic stroke, doctors focus on stopping the bleeding, controlling blood pressure, and preventing complications.
Hospital Care and Acute Phase
In the hospital, you receive continuous monitoring of your heart, blood pressure, oxygen levels, and brain function. Blood tests help doctors understand what caused the stroke and guide prevention of future strokes. CT or MRI scans show exactly where the stroke occurred and its severity. Depending on the type of stroke, you may receive medications to prevent future clots, manage blood pressure, reduce swelling, or prevent seizures.
Doctors also begin evaluating your ability to swallow, as some stroke survivors have difficulty swallowing temporarily. Speech and occupational therapists assess your needs early. Physical therapy may begin almost immediately, even while you are still in the hospital. Early movement and therapy support better recovery outcomes.
Rehabilitation: The Path to Recovery
The most important phase of stroke recovery is rehabilitation. Research clearly shows that rehabilitation therapy significantly improves outcomes and reduces long-term disability, particularly when provided with higher frequency and duration. Many stroke survivors experience their fastest recovery in the first three to six months, though recovery can continue for years.
Physical therapy helps restore movement and strength. Therapists guide you through exercises that retrain your nervous system and help your brain learn new pathways to control movement. What begins as assisted movement progresses to independent movement as your brain relearns how to coordinate your body. Repetition is key—the more you practice, the stronger these new neural pathways become.
Occupational therapy teaches you how to perform daily activities again—eating, dressing, bathing, toileting, and eventually returning to work or hobbies. Speech therapy addresses communication difficulties and swallowing problems. Psychologists help address emotional changes and depression, which are common after stroke.
The Encouraging Reality of Stroke Recovery
The most important message is this: recovery after stroke is real and achievable. Many stroke survivors regain significant function and independence. Your individual recovery depends on the location and severity of the stroke, your age and overall health before the stroke, and how much rehabilitation you receive. However, age alone does not determine recovery—people in their 80s and beyond have made remarkable recoveries with dedicated rehabilitation.
Your brain’s neuroplasticity—its ability to reorganize and form new pathways—is central to recovery. When one area of your brain is damaged by stroke, other areas can learn to take over those functions. This is why rehabilitation works. Through repetitive practice and guided therapy, your brain literally rewires itself. What seems impossible weeks after a stroke often becomes possible with consistent effort and time.
Living Well After Stroke
As you recover, life gradually normalizes. Many stroke survivors return to work, continue hobbies with modifications, travel, and live fully independent lives. Others may have lasting effects but learn to adapt and maintain independence through assistive devices and strategies. The key is rehabilitation, perseverance, family support, and hope.
Preventing another stroke is crucial, as one in four stroke survivors will have another stroke. Managing your blood pressure, taking medications as prescribed, eating a healthy diet, exercising regularly, not smoking, managing diabetes, maintaining healthy weight, and reducing stress all dramatically lower your stroke risk.
Why You Should See a Neurologist
A neurologist specializes in brain and nervous system disorders and is the right specialist for stroke care. Neurologists determine the exact type and location of your stroke, order appropriate tests and imaging, prescribe medications, coordinate rehabilitation services, manage complications, and guide your long-term recovery and prevention strategy. They understand the recovery process and can set realistic expectations based on your specific stroke.
You should see a neurologist immediately if you experience any stroke symptoms, if you have had a TIA, if you have multiple stroke risk factors, or if you have had a stroke and need guidance on recovery and prevention.
Frequently Asked Questions About Stroke
How quickly do I need to get to the hospital?
Immediately. Call 911 at the first sign of stroke symptoms. Every minute matters. Treatment is most effective when started within the first few hours. Do not wait to see if symptoms improve on their own. Rapid medical intervention saves brain tissue and improves outcomes.
Can a stroke be prevented?
Yes. Approximately 80% of strokes are preventable through managing risk factors. Controlling blood pressure, managing diabetes, stopping smoking, eating a healthy diet, exercising regularly, limiting alcohol, maintaining healthy weight, and managing stress all reduce stroke risk significantly.
What is a TIA and how serious is it?
A TIA (transient ischemic attack) is a temporary stroke where symptoms resolve within hours. Although temporary, it is a serious warning sign that you are at high risk for a full stroke. After a TIA, you should see a neurologist urgently to identify the cause and prevent a major stroke.
Will I fully recover from my stroke?
Recovery varies greatly depending on the type and severity of stroke, the areas of the brain affected, your age and health, and the intensity of your rehabilitation. Many people recover significantly and regain independence. Recovery continues beyond the first few months, with some improvement possible for years. The amount and intensity of rehabilitation greatly influences outcomes.
How long does stroke rehabilitation take?
Recovery is a long-term process. The first three to six months typically show the fastest progress. However, meaningful recovery can continue for years with dedicated rehabilitation. Most people continue therapy for weeks to months in the hospital and rehabilitation center, followed by outpatient therapy that may continue for years.
Can I go back to work after a stroke?
Many stroke survivors return to work, though the timeline varies greatly. Some return within weeks or months, while others may need more time or may return with modifications. Work demands affect the timeline—desk work may be possible sooner than physical labor. Discuss your specific situation with your neurologist.
What does rehabilitation therapy actually do?
Rehabilitation therapy retains your nervous system through repetitive practice of movements and tasks. Your brain's neuroplasticity allows other areas to learn to take over functions from the damaged area. Therapy teaches you compensation strategies, helps you regain lost abilities, and helps you adjust to any permanent changes.
Will I have lasting effects from my stroke?
The lasting effects depend on your specific stroke. Some people recover completely. Others have lasting weakness, vision changes, speech difficulties, or cognitive changes. Even when complete recovery does not occur, many people adapt and live independently with assistive devices and strategies.
Can depression happen after a stroke?
Yes, depression is very common after stroke, affecting about one-third of stroke survivors. It is treatable through therapy and sometimes medication. If you feel persistently sad, hopeless, or lose interest in activities, tell your doctor. Treatment can significantly improve mood and support better recovery.
How can I prevent another stroke?
Take medications as prescribed, manage your blood pressure, eat a healthy diet, exercise regularly, stop smoking, manage diabetes, maintain healthy weight, reduce stress, get good sleep, and have regular medical check-ups. These steps reduce your risk of another stroke significantly.
What can family members do to help?
Family support is crucial. Help with transportation to appointments, encourage rehabilitation exercises, provide emotional support, help with daily activities as needed, learn about stroke to understand what your loved one is experiencing, and celebrate progress, even small progress. Your presence and encouragement make a real difference in recovery.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you or someone near you is experiencing stroke symptoms, call 911 immediately.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
