Neuropathy and Myopathy
Neuropathy and Myopathy: Understanding Nerve and Muscle Diseases and Recovery
Numbness, tingling, weakness, or muscle pain can be frightening, but the encouraging reality is that many cases of neuropathy and myopathy are manageable and sometimes reversible. With proper diagnosis, targeted treatment, and rehabilitation, many people regain function and improve significantly. This page explains what neuropathy and myopathy are, what causes them, how they are diagnosed, and what treatments and management strategies are available. It is for education only and does not replace advice from your own doctor.
Understanding Neuropathy
Neuropathy refers to damage to one or more peripheral nerves that leads to weakness, numbness, tingling, burning pain, or other problems in different parts of the body, often beginning in the hands or feet. Peripheral nerves carry signals from your brain and spinal cord to the rest of your body, controlling movement and providing sensation. When these nerves are damaged, these signals become disrupted.
There are different types of neuropathy based on which nerves are affected. Sensory neuropathy affects nerves that carry sensation like touch and temperature, causing tingling, numbness, or burning pain. Motor neuropathy affects nerves that control muscle movement, causing weakness and loss of coordination. Autonomic neuropathy affects nerves that control internal body functions like heart rate, blood pressure, and digestion. Most commonly, people experience combination neuropathy affecting multiple types of nerves at once.
Understanding Myopathy
Myopathy is a disease of the muscles themselves, not the nerves controlling them. With myopathy, the muscle fibers weaken, become inflamed, or deteriorate, leading to progressive weakness and difficulty with movement. Unlike neuropathy where the problem is in the nerves, myopathy is a primary muscle problem.
Common types include muscular dystrophies (genetic muscle-wasting diseases), myositis (inflammatory muscle diseases where the immune system attacks muscles), and metabolic myopathies (muscle diseases related to metabolic problems). Each type has different causes and progression patterns, but all result in muscle weakness and dysfunction.
Key Differences Between Neuropathy and Myopathy
While both neuropathy and myopathy cause weakness, they affect different parts of the nervous system and have distinct characteristics. In neuropathy, weakness typically starts in the hands and feet (distal weakness) and often progresses upward. Sensation is commonly affected—you may experience numbness, tingling, or burning pain. Reflexes are lost early in the disease. In myopathy, weakness typically affects the shoulders, hips, and trunk (proximal weakness) rather than the hands and feet. Sensation is usually preserved—you feel normal touch and temperature. Reflexes are typically preserved until late in the disease.
These differences help doctors determine whether you have neuropathy or myopathy and guide treatment decisions accordingly.
Common Causes of Neuropathy
Diabetes is the most common cause of neuropathy, affecting more than half of all people with diabetes. High blood sugar damages nerve fibers over time, leading to diabetic neuropathy. Other common causes include vitamin B deficiencies (especially B12), particularly in people with poor nutrition or certain medical conditions. Infections such as HIV, hepatitis B and C, and shingles can damage nerves. Autoimmune diseases like lupus, Sjögren’s syndrome, and Guillain-Barré syndrome cause the immune system to attack nerves.
Additional causes include chemotherapy and certain other medications that damage nerves, long-term alcohol abuse leading to vitamin deficiencies, heavy metal or toxin exposure, pressure on nerves from tumours or repetitive activities, and spinal injuries. Sometimes a specific cause cannot be identified, which is called idiopathic neuropathy. Importantly, identifying the underlying cause is crucial because treating it can stop progression and sometimes reverse neuropathy.
Common Causes of Myopathy
Inflammatory myopathies occur when the immune system attacks muscle fibers, including conditions like dermatomyositis and polymyositis. Genetic muscular dystrophies are inherited muscle diseases that cause progressive weakness. Metabolic myopathies result from problems with how muscles generate energy. Toxic myopathies can result from medications like steroids used long-term or from drug abuse. Infections, thyroid problems, and nutritional deficiencies can also cause myopathy.
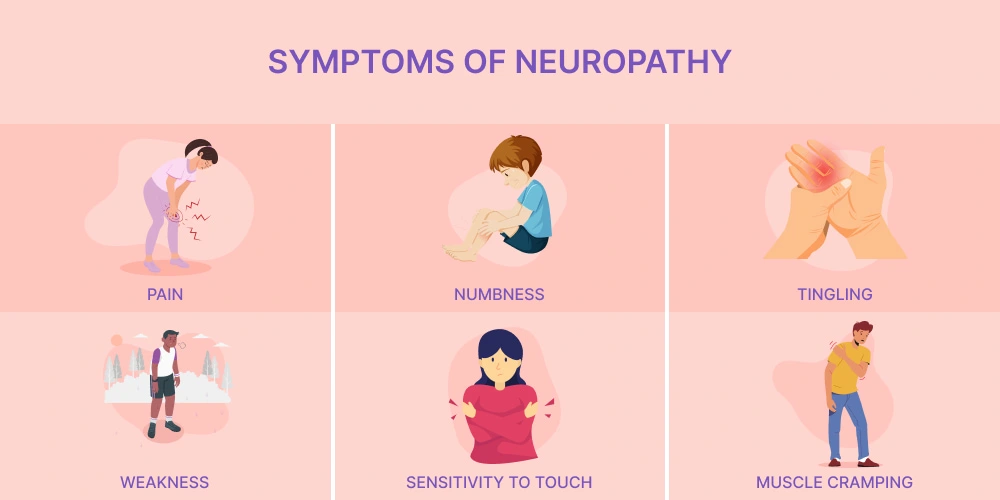
Recognizing Neuropathy Symptoms
Symptoms vary depending on which nerves are affected. Sensory symptoms include tingling or “pins and needles” sensation, numbness especially in hands and feet, burning pain or electric shock-like sensations, and extreme sensitivity to touch. Motor symptoms include weakness in legs or hands, difficulty walking, muscle cramps or twitching, and loss of coordination or balance. Autonomic symptoms include dizziness or lightheadedness, digestive problems or constipation, excessive sweating or inability to sweat, and heart palpitations or irregular heartbeat.
Symptoms often start in the feet and gradually progress upward. Many people describe the sensation as wearing an invisible sock or glove where they cannot feel properly.
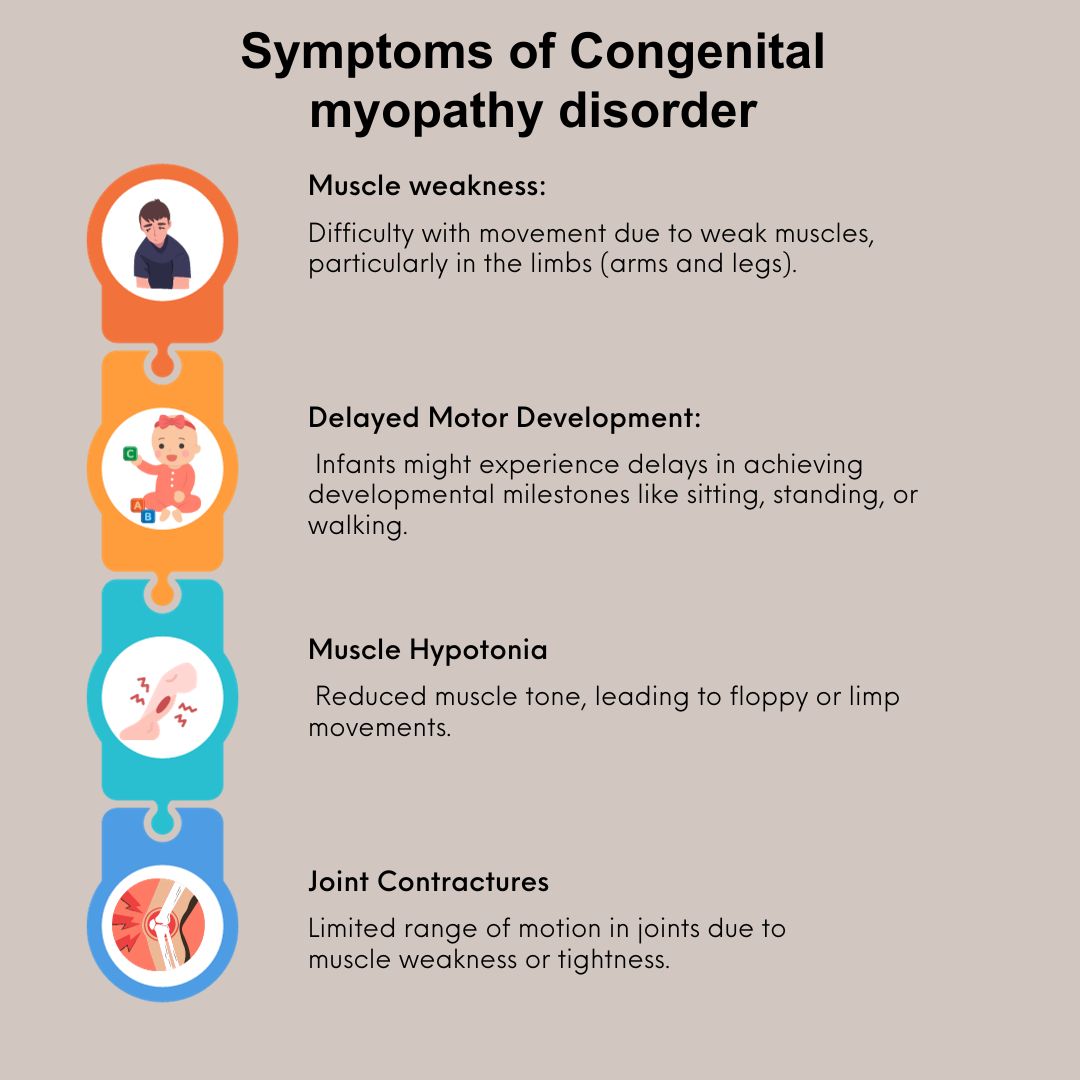
Recognizing Myopathy Symptoms
Myopathy symptoms typically include progressive muscle weakness, particularly in the shoulders, hips, and neck. You may have difficulty climbing stairs, rising from a chair, or lifting your arms above your head. Muscle pain, soreness, or stiffness may accompany weakness. Some people experience muscle cramps or spasms. With inflammatory myopathies, a characteristic rash may appear on the eyelids or knuckles. Difficulty swallowing or shortness of breath can occur if the throat or chest muscles are affected.
The progression varies—some myopathies develop slowly over years, while others progress more rapidly. Unlike neuropathy, sensation is typically normal in myopathy.
When to Seek Medical Attention
See a doctor if you experience persistent numbness, tingling, or burning sensations, progressive muscle weakness, difficulty with balance or walking, or symptoms that interfere with daily activities. Seek urgent evaluation if symptoms appear suddenly, if weakness is severe or rapidly worsening, if you have difficulty breathing or swallowing, if symptoms follow a recent infection or vaccination, or if you have signs of nerve damage after an injury. Early diagnosis and treatment can slow progression and sometimes reverse symptoms, particularly for neuropathies caused by treatable conditions.
How Neuropathy and Myopathy Are Diagnosed
Your doctor begins with detailed questions about when symptoms started, which body parts are affected, whether sensation is affected, whether symptoms are progressing, and whether there is family history of these conditions. They perform a physical examination, testing your strength, sensation, reflexes, and balance.
Blood tests help identify common causes like diabetes, vitamin deficiencies, infections, and immune problems. Nerve conduction studies measure how well electrical signals travel along nerves, helping determine if nerves are damaged. Electromyography (EMG) measures electrical activity in muscles, distinguishing between nerve problems and muscle problems. MRI scans may show muscle inflammation or damage. Muscle biopsy, where a small sample of muscle tissue is examined under a microscope, can diagnose myopathy types.
Treatment for Neuropathy
Treatment focuses on addressing the underlying cause and managing symptoms. If diabetes is the cause, strict blood sugar control can slow progression and sometimes reverse early neuropathy. Treating vitamin deficiencies through supplementation can improve symptoms significantly. Treating infections with appropriate medications stops nerve damage.
Medications that help manage symptoms include pain relievers, medications for nerve pain like gabapentin or pregabalin, topical creams for localized pain, and medications for autonomic symptoms. Physical therapy helps maintain muscle strength and improves balance and coordination, reducing fall risk. Managing blood pressure, eating a healthy diet, exercising regularly, avoiding alcohol, and maintaining healthy weight all support nerve health and prevent progression.
Treatment for Myopathy
Treatment depends on the type of myopathy. For inflammatory myopathies, medications that suppress the immune system, such as corticosteroids, methotrexate, or mycophenolate, reduce muscle inflammation and preserve function. Some newer treatments use intravenous immune globulin or other immunosuppressive approaches. Physical therapy is crucial and should be started early, as research shows that exercise and physical therapy reduce inflammation, increase muscle strength, improve aerobic capacity, and increase stamina even in people with myositis.
Occupational therapy helps adapt activities of daily living. Assistive devices support function and safety. Genetic myopathies currently have limited specific treatments, but physical therapy helps maintain function as long as possible. The key message is that even in conditions without specific cures, treatment significantly improves function and quality of life.
Rehabilitation and Recovery
Physical rehabilitation is essential in both neuropathy and myopathy. In neuropathy, physical therapy improves balance, reduces fall risk, maintains muscle function, and helps you adapt to any remaining symptoms. In myopathy, physical therapy strengthens unaffected muscles, preserves joint mobility, prevents contractures, and maintains aerobic fitness.
For myositis, strengthening programs can begin within 2-3 weeks from the acute phase, progressing from passive range of motion exercises to active strengthening as strength improves. The key is finding the right exercise level—challenging enough to maintain and improve function, but not so intense that it causes harm.
Living Well With Neuropathy or Myopathy
Many people with neuropathy manage symptoms effectively and maintain quality of life with appropriate treatment and lifestyle modifications. Some recover completely, particularly when the underlying cause is treated early. Others experience improvement but may have some residual symptoms. Assistive devices like braces, canes, or walkers help maintain mobility and safety. Adaptive techniques and equipment allow you to continue activities with modifications.
For myopathy, outcomes vary by type. Some genetic myopathies progress slowly over decades, allowing many years of productive life. Inflammatory myopathies often stabilize or improve with treatment. The goal is to maintain the best possible function and independence through appropriate treatment, consistent rehabilitation, and lifestyle adaptation.
Why You Should See a Neurologist
A neurologist specializes in nervous system and neuromuscular disorders and is the right specialist for evaluating neuropathy and myopathy. Neurologists can determine the exact type and cause of your condition, order appropriate tests, manage complex cases, and recommend evidence-based treatments. They coordinate your care with other specialists as needed and can help you access clinical trials for new treatments.
You should see a neurologist if you have symptoms suggesting neuropathy or myopathy, if your condition is not improving with current treatment, if symptoms are progressing rapidly, if you have a family history of these conditions, or if you need guidance on managing a complex case.
Frequently Asked Questions About Neuropathy and Myopathy
Can neuropathy be reversed?
Some types can be reversed, especially if caught early and the underlying cause is treated. Neuropathy from diabetes, vitamin deficiencies, or certain infections can improve significantly with treatment. Other types improve with time and may not reverse completely but can stabilize.
Is neuropathy always progressive?
Not necessarily. Many people with treated neuropathy stabilize and do not worsen further. Some improve over time with proper management. Progressive neuropathy is more common when the underlying cause is not addressed.
Can myopathy be cured?
Cure depends on the type. Inflammatory myopathies often respond well to treatment and can go into remission. Genetic myopathies currently cannot be cured but can be managed to maintain function. New treatments under development show promise.
Will I lose my mobility?
With appropriate treatment and rehabilitation, many people maintain or regain mobility. Some may need assistive devices, but assistive devices extend independence rather than limit it. The key is early diagnosis and treatment.
How much exercise should I do?
This depends on your specific condition. Physical therapists tailor exercise programs to your particular disease and current function. Too little exercise can lead to deconditioning, while too much can be harmful. Work with a therapist to find the right balance.
Can diet help neuropathy?
A healthy diet rich in B vitamins, particularly B12, supports nerve health. Limiting alcohol and avoiding smoking prevent further damage. Managing blood sugar if diabetic is crucial. These lifestyle factors significantly impact progression.
Are there clinical trials available?
Yes, research is ongoing for both neuropathy and myopathy. Ask your neurologist about clinical trials studying new treatments for your specific condition. Trials may offer access to promising new therapies.
Can stress worsen these conditions?
Stress can worsen symptoms by increasing muscle tension and affecting pain perception. Stress management through relaxation, meditation, exercise, or counselling helps manage symptoms.
Will medication help my pain?
Many medications are effective for nerve pain. Options include gabapentin, pregabalin, duloxetine, and topical treatments. If one medication does not work, others can be tried. Pain management often requires trying multiple approaches.
How often should I see my doctor?
This depends on your condition's stability and severity. Initial diagnosis may require frequent visits, but once stable, many people see their neurologist every 3-6 months. Those with rapidly progressing conditions need more frequent monitoring.
Can I work with neuropathy or myopathy?
Many people continue working, especially in desk jobs or roles with flexibility. Some may need workplace modifications or accommodations. Your specific limitations and job demands determine what is possible.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you are experiencing symptoms of neuropathy or myopathy, seek medical evaluation promptly.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
