Encephalitis
Encephalitis: Recognizing Types, Understanding Recovery, and Rebuilding Life
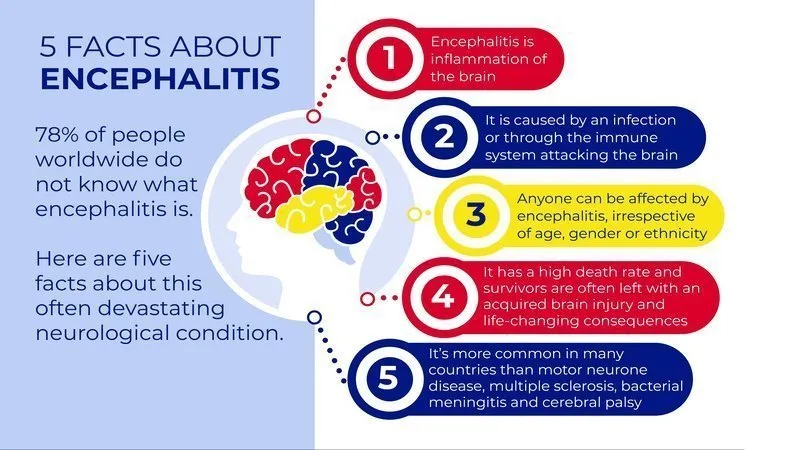
Encephalitis is a serious brain inflammation that can affect anyone at any age, but with proper understanding of the different types and comprehensive care, most people experience meaningful recovery and regain independence. While the acute phase can be frightening, research shows that favorable outcomes are achieved in most patients, and with targeted rehabilitation and support, people rebuild their lives successfully. This page explains the different types of encephalitis, what causes them, how they are treated, and what recovery and long-term life look like. It is for education only and does not replace advice from your own doctor.
Understanding Different Types of Encephalitis
Encephalitis refers to brain inflammation caused by infection or an autoimmune response where the immune system mistakenly attacks the brain. Understanding which type you have is crucial because different types require different treatments and have different recovery trajectories.
Infectious encephalitis occurs when viruses, bacteria, parasites, or fungi invade the brain and trigger inflammation. Viral encephalitis is most common, with causes including herpes simplex virus, West Nile virus, Japanese encephalitis virus, and other arboviruses transmitted by mosquitoes. Autoimmune encephalitis is a distinct type where the body’s immune system mistakenly produces antibodies against the brain’s own proteins. Common forms include anti-NMDA receptor encephalitis and anti-LGI1 encephalitis. These are increasingly recognized and diagnosed types that were previously misdiagnosed as psychiatric conditions or other neurological diseases.
The distinction matters because autoimmune forms often respond dramatically to immunotherapy, while the treatment approach for infectious encephalitis differs based on the specific agent causing infection.
Autoimmune Encephalitis: A Growing Recognition
Autoimmune encephalitis has been increasingly recognized as a treatable neuropsychiatric condition, with advances in diagnostic testing allowing identification of specific antibodies causing the inflammation. This is important because many people with autoimmune encephalitis were previously diagnosed with psychiatric illness, personality disorders, or other conditions and treated ineffectively.
Anti-NMDA receptor encephalitis is one of the most common forms and presents with distinctive psychiatric and neurological features that often develop in young adults, particularly females. Interestingly, autoimmune encephalitis can develop after viral infections like herpes simplex encephalitis, where the initial viral infection triggers development of antibodies that persist and cause ongoing encephalitis. Post-viral autoimmune complications occur in approximately 20% of people who initially recover from viral encephalitis, with some later developing relapsing autoimmune encephalitis.
Recognizing Encephalitis Symptoms
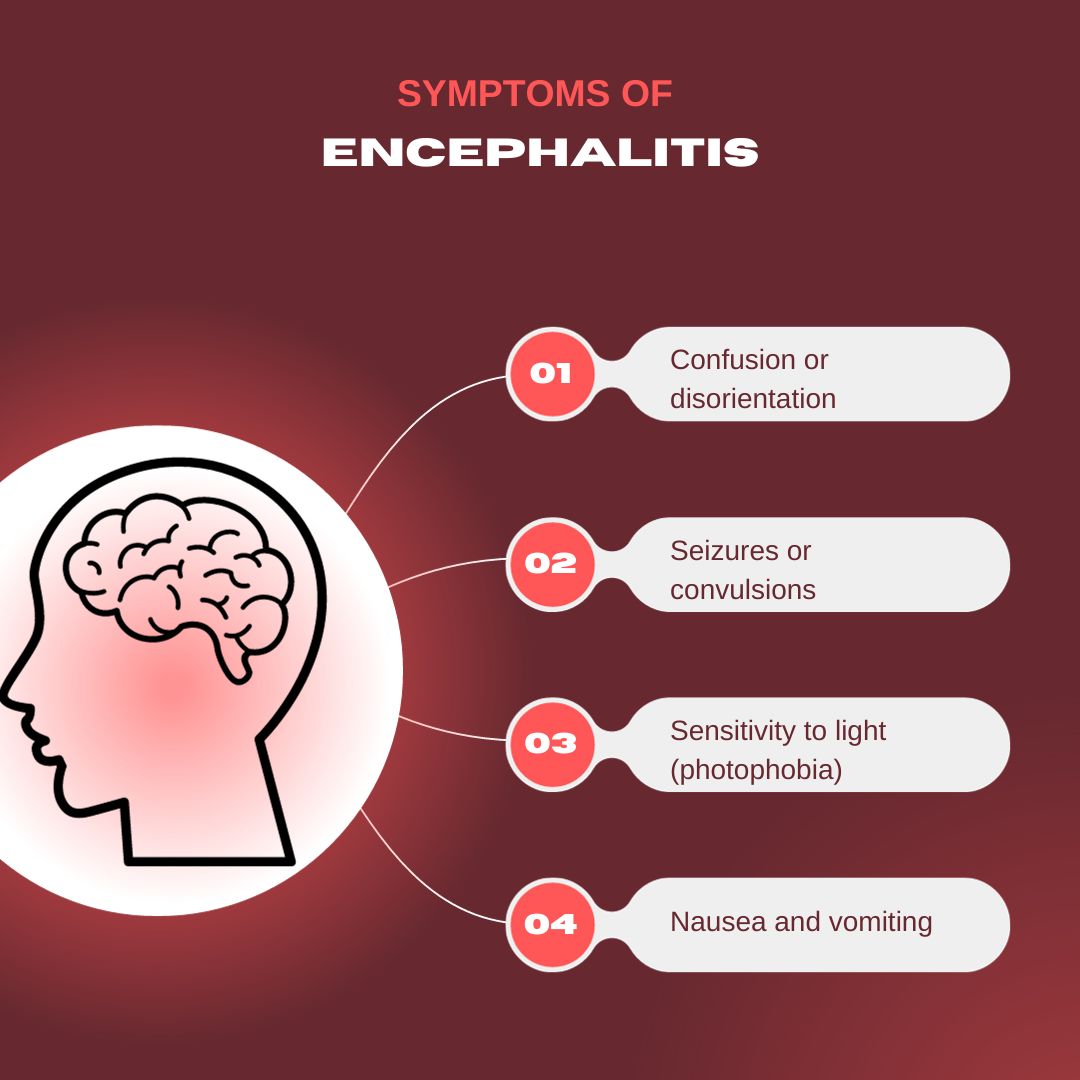
Encephalitis typically begins with prodromal symptoms—signs that precede the main illness. About 70% of patients experience initial headache, fever, and symptoms resembling viral illness before progressing to more severe neurological symptoms. This early phase is sometimes missed, but recognizing it helps with early diagnosis.
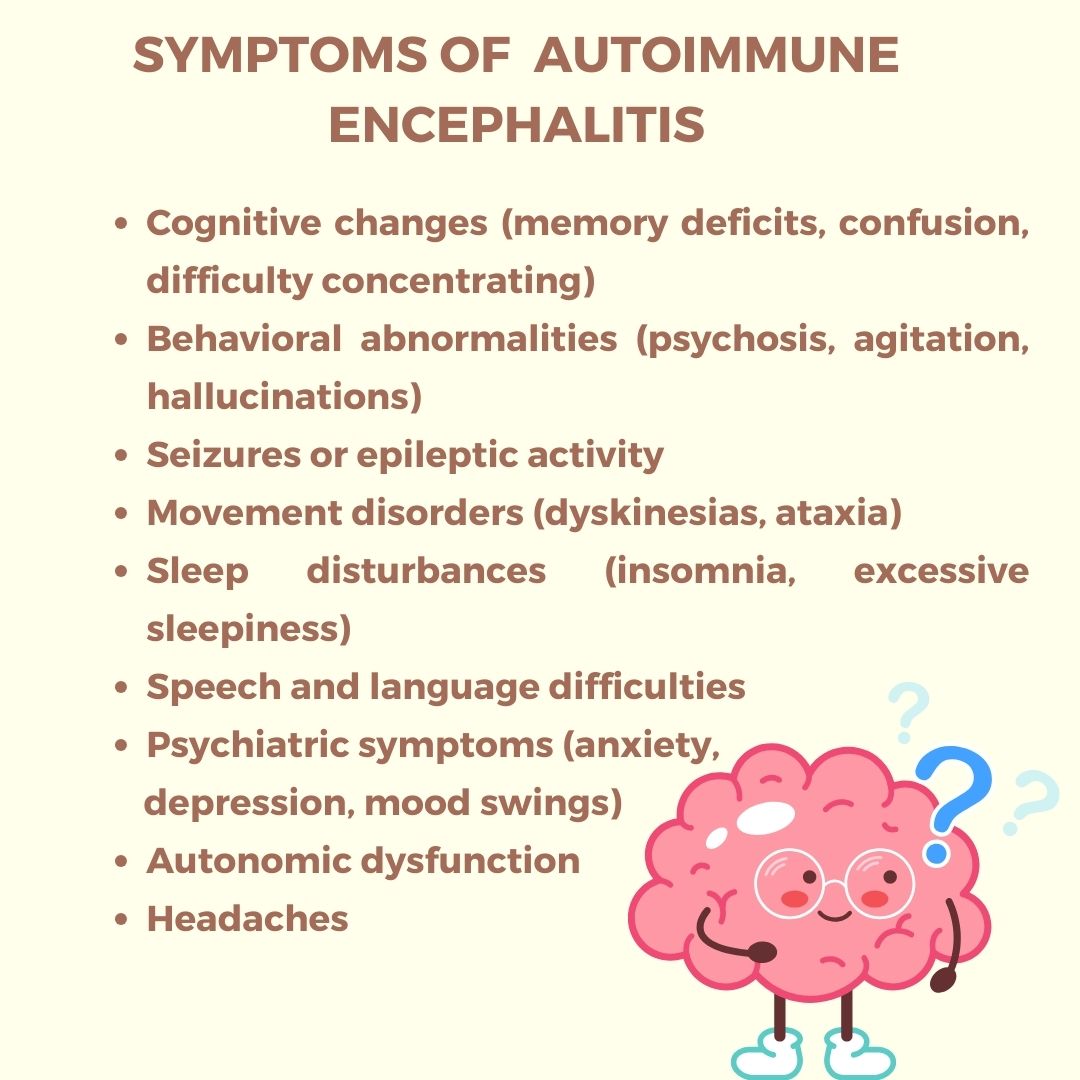
As encephalitis develops, symptoms escalate to include confusion or altered mental status, memory loss or difficulty forming new memories, personality changes or unusual behavior, hallucinations or delusions, agitation or irritability, seizures, movement abnormalities or unusual involuntary movements, and in severe cases, loss of consciousness. The onset can vary from acute over hours or subacute over days to weeks, with a sometimes fluctuating course where symptoms vary in intensity.
Psychiatric symptoms are often the most prominent features, particularly in autoimmune encephalitis. People may experience severe anxiety, paranoia, personality changes, or be mistakenly thought to have psychosis or a psychiatric emergency before the neurological basis is recognized.
When to Seek Emergency Care
Seek emergency care immediately if you or someone near you experiences severe headache with high fever, confusion or significant memory problems, behavioral changes or personality shifts, hallucinations or delusions, loss of consciousness, seizures, or rapid worsening of any neurological symptoms. These symptoms warrant urgent hospitalization and evaluation because early diagnosis and treatment dramatically affect outcomes.
It is particularly important to recognize encephalitis early in autoimmune cases because delays in diagnosis and treatment can result in severe complications including refractory seizures, coma, and potentially reversible brain damage. Early treatment offers substantially better prognoses.
Diagnosis: Finding the Cause Matters
Accurate diagnosis requires multiple tests because determining whether encephalitis is infectious or autoimmune changes treatment significantly. Lumbar puncture testing examines cerebrospinal fluid for signs of infection or inflammation and may show specific markers suggesting autoimmune disease. Brain imaging with MRI shows inflammation patterns and may suggest specific types. Blood and cerebrospinal fluid tests look for viruses, bacteria, or specific antibodies.
Critically, specific antibody testing distinguishes between different autoimmune encephalitis types, allowing targeted immunotherapy rather than general treatment. This is why comprehensive diagnostic evaluation at specialized centers improves outcomes—they have expertise recognizing autoimmune encephalitis and ordering appropriate antibody panels.
Treatment Approaches
Treatment depends on the encephalitis type. Infectious encephalitis is managed with antivirals (for viral), antibiotics (for bacterial), or other agents based on the identified cause. Autoimmune encephalitis responds to immunotherapy including corticosteroids, intravenous immunoglobulins, plasmapheresis, and in some cases rituximab or other immunosuppressive medications. Early immunotherapy is crucial—patients receiving prompt treatment have significantly better outcomes than those with delayed treatment.
Symptomatic treatment addresses specific problems like seizures, movement disorders, behavioral issues, and autonomic dysfunction. Many patients require intensive care monitoring. As acute symptoms improve, rehabilitation begins.
Recovery: A Gradual Process With Variable Timelines
Most patients with encephalitis experience favorable outcomes, meaning they achieve functional independence measured on the modified Rankin Scale. However, the path to recovery is variable and requires patience. Immediate recovery after acute hospitalization may show rapid improvement as inflammation decreases. Middle-phase recovery over weeks to months continues functional improvement. Long-term recovery extends for months to years, with research showing recovery can continue up to 36 months from disease onset.
For autoimmune encephalitis specifically, outcomes continue to improve up to 18 months from symptom onset, with early treatment and avoiding ICU admission as positive prognostic factors. This extended recovery window means that improvement is possible even when initial recovery seems plateaued.
Long-Term Effects: The Hidden Challenge
An important reality is that while most people regain functional independence (ability to care for themselves), many experience persistent long-term effects affecting quality of life. About 80% of patients with anti-NMDAR encephalitis experience persistent cognitive impairments, particularly in memory and language, even while achieving functional independence. Additionally, approximately 43% of encephalitis survivors have neuropsychiatric sequelae including cognitive difficulties, mood changes, sleep problems, or behavioral issues.
These challenges often have greater impact on daily life than might be expected from outward functional recovery. About 30% of patients do not resume work or education, with cognitive processing speed being a key factor determining whether people can return to occupational activities. This highlights that functional independence does not always equal complete recovery or normal quality of life.
Rehabilitation and Rebuilding
Comprehensive rehabilitation addresses the complexity of recovery. Physical therapy restores movement and strength. Speech and occupational therapy address communication and daily living challenges. Cognitive rehabilitation helps with memory, concentration, and thinking skills. Neuropsychological support addresses mood and behavioral changes. Return to work or education may require adjustments, temporary part-time schedules, or workplace accommodations that support gradual return to normal functioning.
Family involvement in rehabilitation is crucial, as family members learning about encephalitis and its effects can provide informed support during recovery. A person-centered approach recognizing individual needs and capabilities leads to better outcomes than one-size-fits-all rehabilitation.
Managing Relapse and Long-Term Monitoring
An important consideration is that some types of encephalitis can relapse. Anti-LGI1 and anti-CASPR2 associated encephalitis have higher relapse rates than other forms. Surveillance imaging and monitoring for persistent or relapsing symptoms is recommended for at least 4 years after onset in autoimmune encephalitis.
This means ongoing follow-up with your neurologist is important to catch any returning symptoms early and resume treatment promptly if needed. Vigilance about recognizing early signs of relapse—mood changes, cognitive changes, or new symptoms—helps ensure rapid intervention.
Prevention Through Vaccination and Awareness
For certain types of encephalitis, prevention is possible. Japanese encephalitis vaccine is recommended for people living in affected countries or traveling for extended periods to endemic areas, particularly rural areas with high mosquito exposure. The vaccine series is given as two doses spaced 28 days apart, with protection lasting several years.
Mosquito avoidance, protective clothing, and insect repellent reduce risk in endemic areas. The best prevention strategy combines vaccination with mosquito protection measures for travelers in high-risk regions. Planning ahead before travel to endemic areas ensures you have adequate protection.
Quality of Life and Long-Term Adjustment
While the path of encephalitis recovery is challenging, most people rebuild meaningful lives. Some patients achieve excellent recovery with minimal persistent effects, while others learn to manage ongoing challenges while maintaining good quality of life. Key factors in successful long-term adjustment include comprehensive rehabilitation, family and social support, neurologist follow-up, and realistic expectations about recovery.
Many survivors report that while they may not return to exactly how they were before encephalitis, they adapt and build satisfying lives with modifications and support. Connection with other encephalitis survivors provides understanding, practical strategies, and hope for ongoing recovery.
Why You Should See a Neurologist
A neurologist is essential for encephalitis care. They coordinate acute diagnosis and treatment, distinguish between infectious and autoimmune types, order appropriate antibody testing, manage complex acute illness, guide rehabilitation planning, monitor for complications and relapse, and support long-term adjustment and quality of life.
You should see a neurologist if you suspect encephalitis, if you are recovering from encephalitis, if you have persistent symptoms affecting function or quality of life, or if you need guidance on managing relapse risk and long-term follow-up.
Frequently Asked Questions About Encephalitis
How is autoimmune encephalitis different from infectious encephalitis?
Autoimmune encephalitis results from the body's immune system attacking its own brain proteins, while infectious encephalitis results from infection. They present similarly but require different treatments. Autoimmune encephalitis typically responds to immunotherapy, while infectious encephalitis is managed with antivirals, antibiotics, or other antimicrobial agents.
Can encephalitis be completely cured?
Most people achieve functional recovery and return to independence. However, persistent cognitive or behavioral changes may remain. These usually improve over extended rehabilitation but may not completely resolve. The goal is maximal recovery and adjustment to any remaining changes.
How long does recovery from encephalitis take?
Initial recovery often occurs within weeks to months of hospitalization. However, meaningful recovery continues for months to years, with research showing improvement up to 3 years from disease onset. Recovery timelines vary greatly based on severity and type.
Will I have memory problems after encephalitis?
Memory problems are common, affecting about 80% of people with anti-NMDAR encephalitis. However, memory often improves over time with rehabilitation. Some people recover memory function, while others learn strategies to compensate for persistent changes.
Can encephalitis come back?
Some types can relapse, particularly anti-LGI1 and anti-CASPR2 encephalitis. This is why long-term follow-up with a neurologist is important. Ongoing monitoring helps catch any returning symptoms early.
Can I return to work after encephalitis?
Many people do return to work, though about 30% do not resume occupational activities. Return timelines and whether adjustments or reduced schedules are needed depends on individual cognitive effects and job demands.
What does it mean if encephalitis was caused by herpes simplex?
HSV encephalitis is a serious form requiring high-dose IV acyclovir. Importantly, some people develop autoimmune encephalitis after herpes encephalitis. This is why follow-up evaluation is important if symptoms persist after initial recovery from HSV encephalitis.
Should I get a Japanese encephalitis vaccine?
If you live in or travel to endemic areas (parts of Asia and Western Pacific) for extended periods, particularly in rural areas, vaccination is recommended. Short-term urban visitors have low risk, but those spending more than a month in rural areas should strongly consider vaccination.
How do I support someone recovering from encephalitis?
Learn about their specific challenges. Be patient with memory problems or cognitive changes. Encourage rehabilitation participation. Help with adjustments or accommodations needed for return to work or activities. Provide emotional support as they adjust to any persistent effects.
What is the long-term quality of life after encephalitis?
Most people achieve good functional independence and quality of life. However, persistent cognitive or behavioral changes affect some people's daily functioning and work capacity. Realistic expectations, comprehensive rehabilitation, family support, and ongoing neurologist care all contribute to best possible long-term outcomes.
Are there support groups for encephalitis survivors?
Yes, organizations focused on encephalitis provide support groups, educational resources, and connection with others on similar recovery journeys. Connecting with other survivors often provides valuable perspective and practical guidance for navigating recovery.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you suspect encephalitis, seek medical evaluation immediately.
This content does not replace professional medical advice, diagnosis, or treatment. Always seek medical care for suspected encephalitis.
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
