Insomnia
Insomnia: Understanding Sleep Problems, Finding Solutions, and Restoring Rest
Insomnia affects millions of people, robbing them of the sleep they desperately need. But the encouraging reality is that insomnia is very treatable. With the right approach, most people can restore their natural sleep patterns and enjoy restful nights again. This page explains what insomnia is, what causes it, how it is diagnosed, and what effective treatments are available. It is for education only and does not replace advice from your own doctor.
What Is Insomnia?
Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, waking up too early and being unable to return to sleep, or feeling unrefreshed even after a full night in bed. It is one of the most common sleep disorders and affects people of all ages.
Insomnia can be short-term (acute) or long-term (chronic). Short-term insomnia lasting a few days or weeks often occurs with stress, travel, or major life changes and usually resolves on its own. Chronic insomnia, where sleep problems occur at least three times per week for at least three months, requires more targeted treatment but is very responsive to the right interventions.
The key point is this: insomnia does not have to be permanent. Research shows that effective treatments can help people fall asleep faster, stay asleep longer, and wake up feeling truly rested. Many people who struggled with years of sleepless nights have reclaimed their sleep through proper treatment.
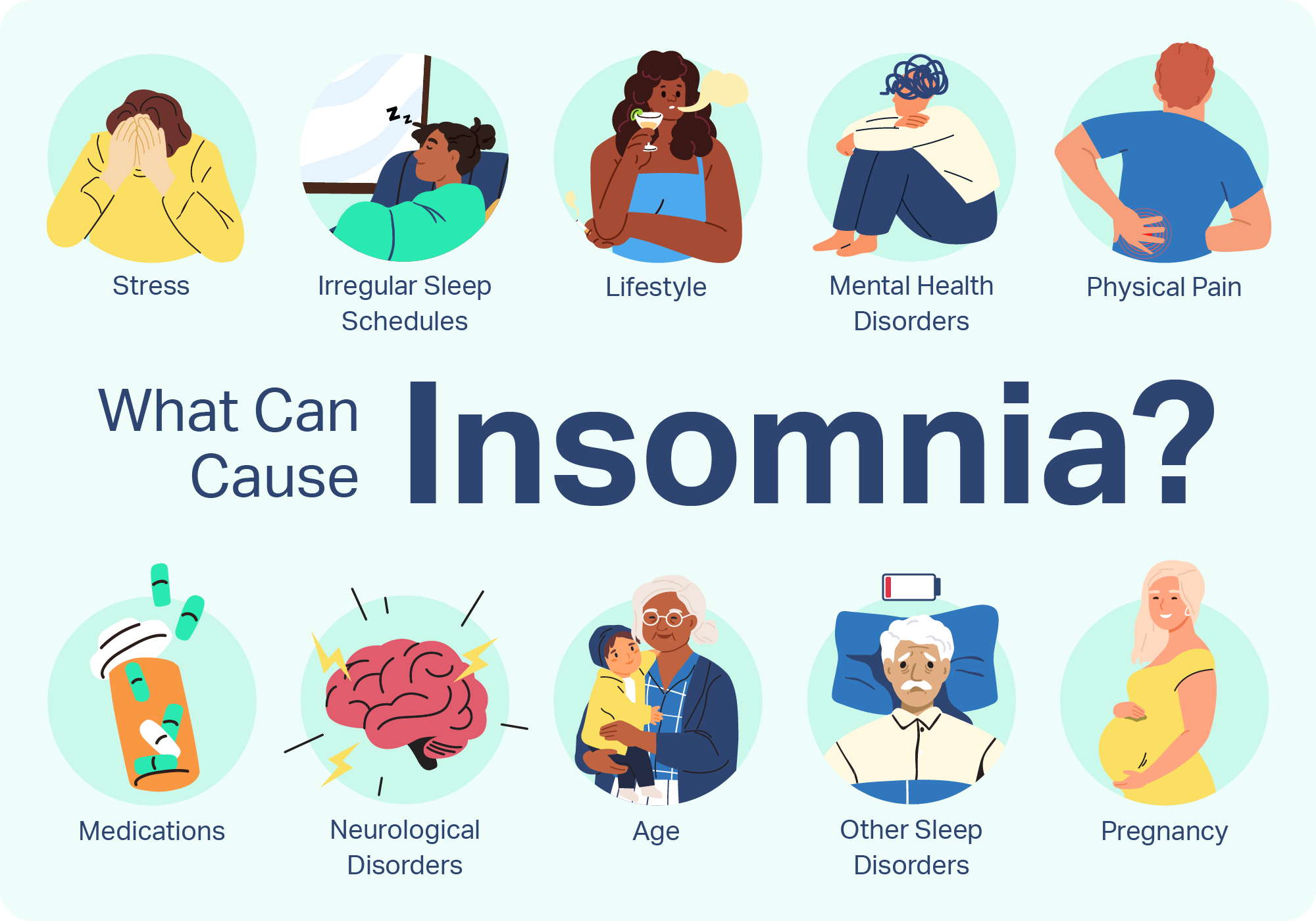
What Causes Insomnia?
Understanding what causes your insomnia is the first step toward solving it. Insomnia can result from stress and anxiety related to work, health, finances, family, or personal relationships. Major life events like illness, job loss, or relationship changes often trigger sleep problems.
Poor sleep habits, also called inadequate sleep hygiene, are a common cause of insomnia. These include irregular sleep schedules, spending too much time in bed, napping during the day, using phones or computers before bed, or consuming caffeine, alcohol, or heavy meals close to bedtime.
Medical conditions can interfere with sleep, including chronic pain, asthma, acid reflux, heart disease, diabetes, Parkinson’s disease, and neurological disorders. Medications used to treat depression, high blood pressure, and certain other conditions can also cause insomnia as a side effect.
Mental health conditions like depression, anxiety, bipolar disorder, and post-traumatic stress disorder commonly cause sleep problems. Your lifestyle also matters—shift work, frequent travel, excessive alcohol consumption, and nicotine use all disrupt sleep patterns.
Recognizing Insomnia Symptoms
The symptoms of insomnia vary from person to person. Some people struggle to fall asleep at all, taking hours to drift off even when exhausted. Others fall asleep easily but wake frequently during the night or very early in the morning and cannot return to sleep.
Beyond the nighttime symptoms, insomnia affects daytime function. People with insomnia often experience fatigue, difficulty concentrating, mood swings, irritability, and difficulty completing daily tasks. Some experience headaches, worry constantly about sleep, or have weakened immune function. This daytime impact is why treating insomnia quickly is important—it affects your entire life, not just nighttime.
When to Seek Medical Attention
Additionally, see a doctor if you snore or gasp for air while sleeping, wake up so many times at night, wake up feeling unrefreshed, or have been unable to concentrate or pay attention due to sleep issues. Early consultation with a healthcare provider is important because insomnia often has treatable underlying causes, and the longer you wait, the more ingrained the sleep problem can become.
Before visiting a sleep specialist, talk with your primary care healthcare professional if sleep issues are significantly impacting your daily life. Your doctor can evaluate whether your insomnia is related to other medical conditions or medications that can be addressed.
How Insomnia Is Diagnosed
Diagnosis of insomnia begins with a detailed conversation between you and your doctor. The specialist will ask about your sleep patterns, when the problem started, what you were doing before it began, what you have tried to treat it, and how it affects your daily life. They will also ask about your work schedule, exercise habits, diet, medications, and any stressful life events.
Your doctor may ask you to keep a sleep diary for one to two weeks, writing down when you go to bed, how long it takes to fall asleep, how many times you wake, how long you sleep, and how you feel the next day. This sleep log provides valuable information about your sleep patterns and helps identify triggers.
Your doctor will perform a physical examination and likely order blood tests to rule out underlying medical conditions like thyroid problems, anemia, or hormonal imbalances. In some cases, a sleep specialist may recommend a polysomnography test (sleep study) where you sleep in a laboratory while equipment monitors your brain waves, heart rate, breathing, and eye movements. This test identifies specific sleep disorders and guides treatment.
Highly Effective Treatment Options
The encouraging news is that insomnia responds well to treatment. Cognitive Behavioral Therapy for Insomnia (CBT-I) is considered the most effective treatment for chronic insomnia and is recommended as the first-line treatment by international health guidelines.
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is a short, structured, evidence-based approach that addresses the thoughts, feelings, and behaviors contributing to insomnia. Unlike sleeping pills that mask symptoms, CBT-I works by retraining your brain and restoring your body’s natural sleep mechanism.
The results are impressive. Research shows that most individuals who try CBT-I experience improvements to their insomnia and better quality sleep, with benefits continuing long after treatment ends. Studies show CBT-I produces results equivalent to sleep medication but with no side effects, fewer relapses, and continued improvement over time.
Relaxation and Behavioral Techniques
Beyond formal CBT-I, several relaxation techniques significantly improve sleep. Practices such as mindfulness meditation, progressive muscle relaxation, guided imagery, deep breathing, gentle stretching, and yoga have been shown to improve sleep quality and reduce anxiety about sleep.
Sleep Medications
When behavioural approaches alone are not sufficient, your doctor may prescribe short-term sleep medications like melatonin, or prescription medications such as benzodiazepine receptor agonists or dual orexin receptor antagonists. These are typically used temporarily to help you sleep while you are learning new sleep habits through CBT-I. Combining medication with behaviour change offers the best results.
Additional Therapeutic Options
Sleep Hygiene: Building Better Sleep Habits
Improving sleep hygiene—your daily sleep habits—is foundational to treating insomnia. Establishing a regular sleep schedule by going to bed and waking up at the same time every day, even on weekends, helps regulate your body’s internal clock.
Avoiding caffeine after early afternoon, limiting alcohol consumption, and not eating large meals close to bedtime all support better sleep. Reducing screen time before bed is important—the blue light from phones, tablets, and computers suppresses melatonin production and keeps your brain stimulated.
Regular exercise during the day improves sleep, but avoid vigorous exercise close to bedtime. Establishing a calming bedtime routine such as reading, listening to calming music, or practicing deep breathing signals to your body that it is time to wind down and prepares you for sleep.
Why You Should See a Sleep Specialist
A sleep specialist is a doctor trained to diagnose and treat sleep disorders and can determine what is causing your specific sleep problem. They can order appropriate tests, prescribe targeted treatments, coordinate therapy, and monitor your progress. Sleep specialists understand the complex relationship between sleep, brain function, and overall health.
You should see a sleep specialist if your insomnia persists despite trying lifestyle changes, if you suspect an underlying sleep disorder like sleep apnea, if your insomnia is severely affecting your work or relationships, or if other doctors have not been able to help. A sleep specialist can create a comprehensive, personalized treatment plan tailored to your specific needs.
Living Well With Better Sleep
Once you begin proper treatment, many people experience dramatic improvements. Regular sleep returns gradually as you practice new habits, restructure unhelpful thoughts about sleep, and allow your body’s natural sleep mechanism to restore itself. Patience during the process is important—while some people see rapid improvement, others may need several weeks of consistent effort.
The benefits extend far beyond nighttime sleep. As sleep improves, you will likely notice better daytime energy, improved mood, sharper thinking, better memory, improved immunity, and better work or school performance. Many people describe feeling like they have their life back once sleep returns to normal.
Frequently Asked Questions About Insomnia
How long does it take to overcome insomnia?
The timeline varies. Some people see improvement within days of starting CBT-I or changing sleep habits. Others need several weeks of consistent effort. With proper treatment, most people experience significant improvement within 4 to 8 weeks. Some continue improving for months as their sleep naturally consolidates.
Is insomnia permanent?
No. Insomnia is very treatable. Even people who have suffered from insomnia for years can regain normal sleep through the right treatment approaches. The brain's ability to relearn healthy sleep patterns is remarkable.
Can I overcome insomnia without medication?
Yes. CBT-I and behavioral approaches are highly effective on their own, often producing results equivalent to medication. Many people overcome insomnia through behaviour change alone. However, short-term medication combined with behavioural therapy can accelerate improvement.
What is the best treatment for insomnia?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is considered the gold standard treatment and is recommended as first-line treatment by international health organizations. It is often most effective when combined with improved sleep hygiene and sometimes short-term medication.
Why does my mind race at night?
Racing thoughts at night usually result from stress, anxiety, or being in a sleep-deprived state where your brain is overactive. CBT-I teaches techniques to quiet your mind. Relaxation practices and stress management also help significantly.
Is it OK to use my phone in bed?
No. The blue light from phones suppresses melatonin production and keeps your brain stimulated. Additionally, associating your bed with phone use weakens the connection between bed and sleep. Keep phones out of the bedroom or at minimum put them away 30-60 minutes before sleep.
How many hours of sleep do I need?
Most adults need 7 to 9 hours of sleep per night. However, the amount varies by individual. Focus on how rested you feel rather than hitting a specific hour target. If you consistently feel refreshed after 7 hours, that is your need. If you still feel tired, you may need more.
Will I be dependent on sleep medication forever?
Sleep medications are typically meant for short-term use while you learn new sleep habits through CBT-I. Once your sleep normalizes, medications can usually be gradually discontinued. The goal is to restore natural sleep rather than create medication dependence.
What if my insomnia comes back?
If insomnia returns, the skills you learned through CBT-I remain with you. You can reapply techniques that helped before. Additionally, addressing whatever new stressors or life changes triggered the return of insomnia is important.
Can children have insomnia?
Yes, children can experience insomnia. Causes often include anxiety, poor sleep habits, irregular sleep schedules, or medical conditions. Behavioural approaches work very well for children and are usually the first-line treatment.
Is it normal to worry about sleep?
It is common to worry about sleep, but this worry can actually make insomnia worse, creating a vicious cycle. CBT-I teaches you to reduce sleep-related worry and anxiety, which paradoxically leads to better sleep.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you are experiencing persistent sleep problems, seek medical advice promptly.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
Last Updated: November 2025
More Information & Next Steps
If you are looking for more information or want to discuss your sleep concerns with a specialist, you can use the links below:
