Sciatica / Slipped Disc
Sciatica and Slipped Disc: Understanding Pain, Recovery, and Returning to Activity
Sharp, shooting pain that radiates from your lower back down through your leg can be debilitating. But the encouraging news is that most cases of sciatica and herniated discs improve significantly with proper care and rehabilitation. With the right treatment approach, most people recover completely within weeks to months and return to their normal activities. This page explains what sciatica and slipped discs are, what causes them, how they are diagnosed, and what treatments help you recover. It is for education only and does not replace advice from your own doctor.
Understanding Sciatica
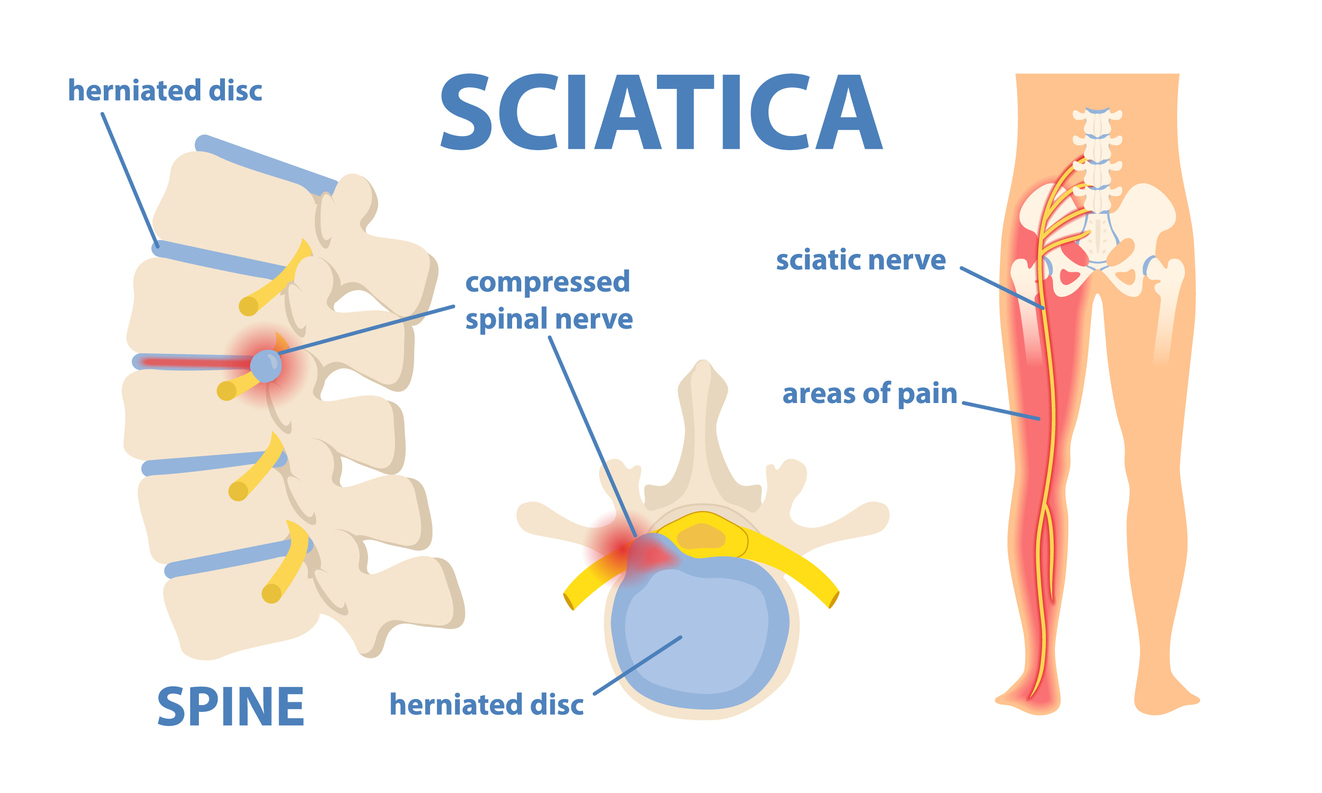
Sciatica is a set of symptoms caused by irritation or compression of the sciatic nerve, the largest nerve in your body. The sciatic nerve starts in your lower spine, travels through your buttock, and branches all the way down into your legs and feet. When this nerve is compressed or irritated, it causes pain, numbness, tingling, or weakness that typically radiates down one leg.
Sciatica is not a disease itself—it is a symptom of an underlying condition pressing on the nerve. The most common cause is a herniated disc in the lower spine. Other causes include spinal stenosis (narrowing of the spinal canal), bone spurs from arthritis, piriformis syndrome (a tight muscle in the buttock), or spondylolisthesis (a slipped vertebra). Understanding the underlying cause is important because it guides treatment decisions.
Understanding Slipped Disc (Herniated Disc)
A slipped disc, medically called a herniated disc, occurs when the soft interior of a spinal disc ruptures or bulges through the tougher outer layer. The spine is made of bones (vertebrae) stacked on top of each other, with discs between them acting as shock absorbers. Each disc has a tough outer shell and a soft gel-like center. When a disc herniates, the inner material pushes into the spinal canal, potentially compressing nearby nerves.
Not all herniated discs cause symptoms. Many people have herniated discs discovered on imaging but experience no pain because the disc material is not pressing on a nerve. When the herniated material does compress a nerve, it causes radiating pain, numbness, or weakness in the area supplied by that nerve. For lower back discs, this often means sciatica.
How Sciatica Develops
The path of the sciatic nerve explains why sciatica pain travels in patterns. Because the nerve is so long and runs down the entire leg, compression at any point along the spine can cause pain anywhere along the nerve’s pathway. This is why some people feel pain only in the buttock, while others feel pain all the way down the leg to the foot and toes.
The pain sensation can vary dramatically. Some people describe sharp, “knife-like” pain, while others experience burning sensations, electric shock-like feelings, numbness, tingling, or weakness. Pain may worsen with certain movements like bending forward, twisting, or straining, and often improves with lying down or changing position. Many people find relief in dark, quiet rooms similar to how migraine sufferers find relief.
Common Risk Factors
Sciatica is surprisingly common, affecting up to 40% of people at some point in their lives. Certain factors increase your risk. Age is a significant factor—you are most likely to develop sciatica between ages 30 and 50, when discs naturally begin to lose water content and become less flexible. Obesity or excess weight places additional stress on the spine and increases the risk of disc problems. Diabetes affects blood sugar metabolism and can increase nerve damage risk. Jobs involving heavy lifting, prolonged sitting, or frequent twisting place stress on the lower back. Being sedentary for long periods also increases risk.
Importantly, many of these risk factors are manageable. Maintaining a healthy weight, staying physically active, practicing good posture, and using proper lifting techniques all reduce your risk significantly.
Recognizing Sciatica Symptoms
Sciatica symptoms vary depending on which nerve root is compressed. The most common symptom is lower back pain or pain in the buttock that radiates down one leg. Pain may be constant or intermittent, and typically affects only one side of the body. Some people experience severe pain, while others have mild discomfort.
Beyond pain, you might experience numbness or tingling, especially in the foot or toes. Weakness in the leg or foot can make walking difficult or cause stumbling. Some people have difficulty controlling their bowel or bladder, which requires urgent medical attention as it suggests cauda equina syndrome, a serious compression requiring emergency care.
It is important to distinguish true sciatica from other leg pain. Hip arthritis causes groin or inner thigh pain, not radiating leg pain. Peripheral neuropathy causes symmetric numbness in both legs, not one-sided radiating pain. Vascular disease causes leg cramps from poor circulation. Getting the right diagnosis matters for receiving appropriate treatment.
How Sciatica and Herniated Discs Are Diagnosed
Your doctor begins by taking a detailed history of your symptoms. When did the pain start? What makes it better or worse? Where exactly does it hurt? Have you had back injuries? This information helps identify potential causes.
Your doctor performs a physical examination, assessing your posture, range of motion, strength, and reflexes. They may perform specific tests like the straight-leg raise test, where you lie on your back and your doctor slowly raises your leg to see if pain reproduces your symptoms. They check for any signs of nerve damage or weakness.
If imaging is needed, MRI scans provide the best view of soft tissue including discs and nerves, while X-rays show bone structure and may reveal arthritis or bone spurs. Sometimes a nerve conduction study or EMG test measures how electrical signals travel along nerves. However, imaging is typically done only if symptoms have not improved after several weeks, as many herniated discs resolve naturally without imaging affecting treatment decisions.
The Encouraging Reality of Recovery
Here is the most important message: most cases of sciatica and herniated discs improve on their own. Research shows that 80 to 90% of patients with sciatica get better over time without surgery, typically within several weeks if the underlying cause is a herniated disc. Further studies demonstrate that 85 to 90% of symptomatic lumbar disc herniations resolve within 6 to 12 weeks without substantial medical intervention.
This recovery happens through natural processes. The body gradually reabsorbs the leaked disc material through phagocytosis and enzymatic processes. Swelling around the nerve gradually decreases, and over time, the compressed nerve is released. Your body has remarkable natural healing abilities for these conditions.
Conservative Treatment: The First-Line Approach
For most people, conservative treatment is all that is needed. Rest is important initially, but complete bed rest is not recommended. Most patients recover through a combination of rest, heat or cold compresses, anti-inflammatory medications (NSAIDs), and then physical therapy. The goal is to manage pain while allowing natural healing.
In the acute phase, ice reduces inflammation and pain, particularly in the first 48 hours. After that, heat therapy relaxes muscles and improves blood flow. Over-the-counter or prescribed pain medications provide relief, allowing you to move more comfortably. Muscle relaxants may help if muscle spasm is significant.
Physical therapy is crucial. Physical therapists use stretching, core strengthening, and specific exercises that rotate the hip to relieve pressure on the sciatic nerve, providing real relief. Starting with gentle movement and gradually progressing to strengthening exercises helps restore function. Maintaining good posture, sleeping on a supportive mattress, and avoiding positions that aggravate pain all support recovery.
Advanced Treatment Options
When conservative treatment provides insufficient relief after several weeks, additional options exist. Epidural steroid injections deliver corticosteroids directly near the irritated nerve, reducing inflammation and providing pain relief that allows physical therapy to be more effective. This is a temporary measure that provides a window for healing and therapy. Oral steroids may be prescribed to reduce overall inflammation.
Nerve blocks, where local anesthetic is injected near the affected nerve, can provide temporary relief. These interventions work best combined with aggressive physical therapy, as addressing the mechanical problem through exercise and strengthening is what leads to lasting recovery.
Surgery: When Conservative Treatment Is Not Enough
Surgery is considered only when conservative treatment has failed or when there is severe, progressive nerve damage. For herniated discs, common procedures include discectomy (removal of the herniated disc portion) or laminectomy (removal of part of the vertebra to relieve pressure). In rare cases of spinal instability, spinal fusion may be performed.
The encouraging news is that when surgery is needed, recovery can be straightforward. Many people experience pain relief immediately or very soon after surgery. However, most people achieve pain relief without surgery through conservative care, which is why surgery is usually a last resort.
Recovery Timeline and Return to Activity
During the first 2-6 weeks, you should expect gradual improvement with decreased pain intensity, reduced muscle spasms, improved range of motion, and less numbness or tingling. Between 6-12 weeks, pain continues improving and you regain strength and mobility. Beyond 12 weeks, most people can resume normal activities, though maintaining good posture, regular exercise, and healthy practices prevents relapse.
During rehabilitation, you progress from passive to active movement. Initially, your physical therapist may guide your movements. Gradually, you perform movements yourself and add resistance. The key is consistency—regular therapy and home exercises are more important than intensity. Returning to activities too quickly can trigger setback, so gradual progression is wise.
Why You Should See a Neurologist
A neurologist specializes in nerve disorders and is the right specialist when sciatica is severe, persistent, or associated with significant nerve damage. Neurologists can determine the exact cause of your sciatica, perform specialized testing if needed, manage complex cases, and coordinate surgical consultation if necessary.
You should see a neurologist if your sciatica is severe or worsening despite conservative treatment, if you have signs of significant nerve damage like severe weakness or loss of bowel/bladder control, if you have recurring sciatica episodes, or if you need guidance on returning to work or activities. A neurologist ensures you receive appropriate care for your specific situation.
Frequently Asked Questions About Sciatica and Slipped Disc
How long does sciatica usually last?
Most people experience significant improvement within 2-6 weeks and complete recovery within 6-12 weeks with proper treatment. Some improve faster, while others take longer depending on severity and individual factors.
Can sciatica go away on its own?
Yes. About 80-90% of people recover without surgery. The body naturally reabsorbs herniated disc material and reduces nerve compression over time. Conservative treatment speeds this process.
Will I need surgery for my sciatica?
Most people will not need surgery. Only when conservative treatment fails after significant time or when there is severe progressive nerve damage is surgery considered. Surgery success rates are good when it is needed.
Can I exercise with sciatica?
Yes, and you should. Gentle movement is better than complete rest. Physical therapy with guided exercises is essential for recovery. Your therapist will recommend appropriate exercises.
What makes sciatica pain worse?
Bending forward, prolonged sitting, twisting, heavy lifting, and coughing or sneezing can worsen pain. Heat, ice, movement, and position changes often provide relief.
Can sciatica be prevented?
Yes. Maintaining healthy weight, regular exercise, good posture, proper lifting technique, and avoiding prolonged sitting all reduce your risk significantly.
Is it OK to rest with sciatica?
Initial rest helps, but bed rest should be limited. Gentle movement, stretching, and physical therapy are more beneficial than prolonged inactivity, which can weaken muscles and slow recovery.
How do I know if I need surgery?
Surgery is considered when conservative treatment provides inadequate relief after several months or when there is significant, progressive nerve damage with weakness or loss of function. Discuss with your neurologist if you might be a candidate.
Are there activities I should avoid?
Avoid heavy lifting, repetitive bending, twisting, prolonged sitting, and activities that reproduce your pain. Most daily activities can continue with modifications.
Can sciatica come back?
Yes, but prevention strategies reduce recurrence risk significantly. Maintaining good posture, regular exercise, healthy weight, and proper lifting technique prevent most recurrences.
How soon can I return to work?
This depends on your job and the severity of your condition. Office work may be possible sooner than physical labor. Discuss with your doctor about modifications needed to return safely.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you are experiencing severe or persistent sciatica symptoms, seek medical advice promptly.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
