Vertigo/Dizziness and Syncope
Vertigo, Dizziness, and Syncope: Understanding Balance, Fainting, and Finding Stability
The world spinning around you, feeling like you might fall, or suddenly losing consciousness are frightening experiences. But the good news is that most cases of vertigo, dizziness, and syncope are highly treatable. With proper diagnosis and management, people regain their stability, confidence, and ability to move freely. This page explains what these conditions are, what causes them, and how they are treated. It is for education only and does not replace advice from your own doctor.
Understanding Vertigo and Dizziness
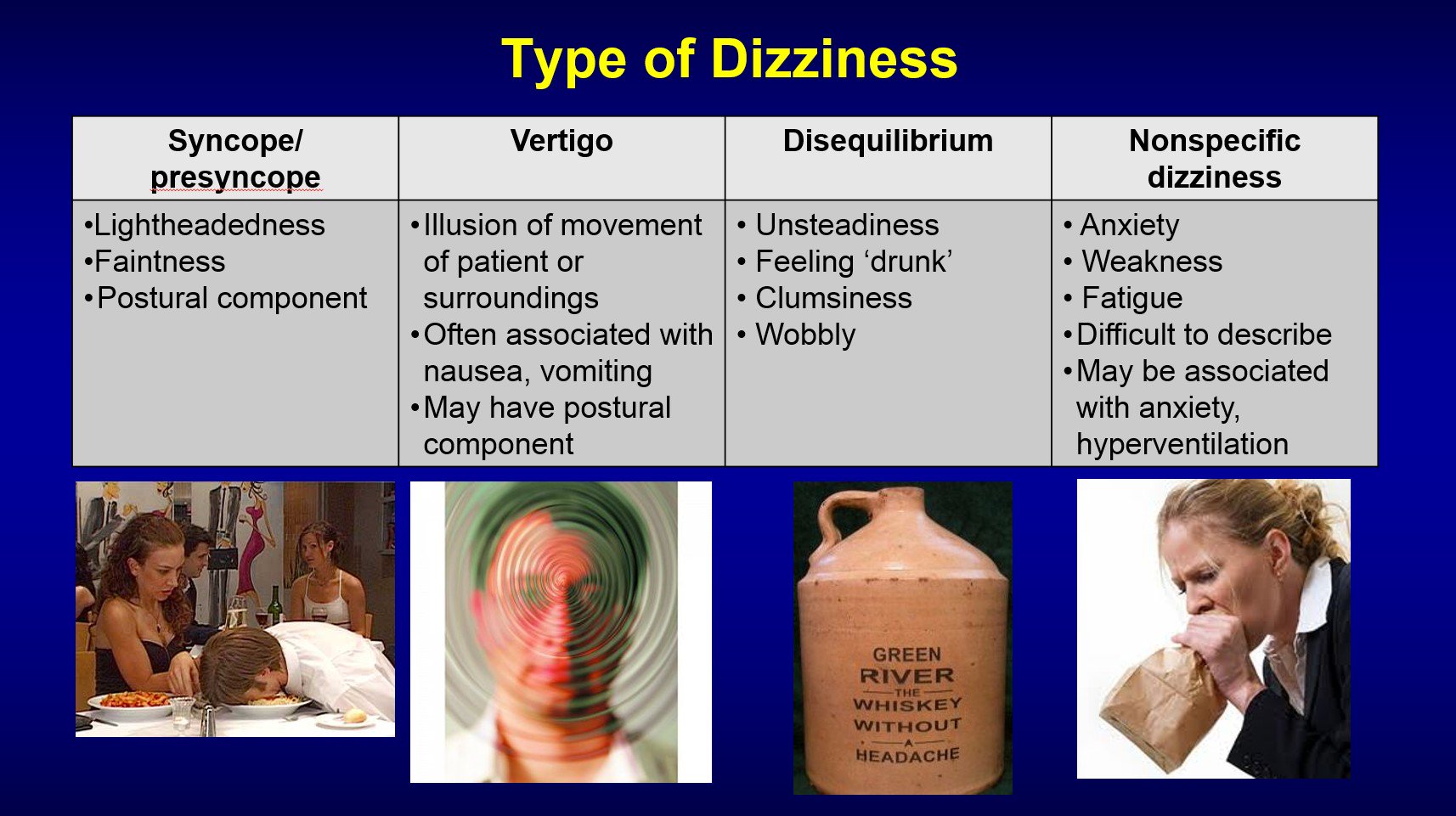
Vertigo and dizziness are different conditions that are often confused. Dizziness is a general term describing feelings of lightheadedness, unsteadiness, weakness, or loss of balance. You feel faint or off-balance but without the sensation of movement. Vertigo, by contrast, is a specific sensation that the room is spinning around you or that you are spinning, even though you are standing still.
Understanding the difference matters because they often have different causes and require different treatments. Dizziness might result from low blood pressure, dehydration, or medications. Vertigo typically relates to your inner ear or balance system. Both conditions can significantly affect daily life, but both respond well to appropriate treatment.
Common Causes of Dizziness
Dizziness can result from many causes, most of which are straightforward to treat. Dehydration is one of the most common causes—not drinking enough water lowers blood pressure and causes lightheadedness. Low blood sugar from skipping meals and blood pressure that drops suddenly when standing up both cause dizziness. Certain medications like blood pressure medicines, antibiotics, or sedatives can cause dizziness as a side effect. Anemia, where your blood lacks enough red blood cells to carry oxygen to your brain, commonly causes lightheadedness.
Anxiety and stress can trigger dizziness. Your inner ear problems, neurological conditions, vision problems, or even motion sickness can all cause feelings of unsteadiness. The key is identifying the underlying cause so it can be properly addressed.
Common Causes of Vertigo
Vertigo most commonly stems from problems with your inner ear and balance system. The inner ear contains structures that sense your head position and movement, sending signals to your brain about balance. When something disrupts this system, vertigo results.
The most common cause of vertigo is Benign Paroxysmal Positional Vertigo, or BPPV. With BPPV, tiny calcium carbonate crystals in your inner ear become dislodged and move around in the fluid-filled canals. This disrupts your balance signals, causing sudden spinning sensations, typically when you move your head or change position. The encouraging news is that BPPV is highly treatable and most patients experience significant relief within a few sessions of treatment.
Other causes of vertigo include infections of the inner ear, inflammation of the vestibular nerve, Meniere’s disease, migraines associated with vertigo, and in less common cases, stroke or brain tumours. Most vertigo cases are from the inner ear and are very manageable.
Symptoms You Should Recognize
Vertigo symptoms include a spinning or rotating sensation, feeling like the room is tilting or moving, loss of balance, nausea or vomiting, and difficulty focusing your eyes. These symptoms can be mild and last seconds, or severe and last hours. Some people experience vertigo only when moving their head a certain way, while others feel it constantly.
Dizziness symptoms include lightheadedness, feeling weak or unsteady, seeing the room sway slightly, and feeling like you might fall. Unlike vertigo, dizziness does not involve a spinning sensation.
When to Seek Medical Attention for Vertigo and Dizziness
Seek medical attention if dizziness or vertigo is new, severe, or interfering with your daily activities. See a doctor if your symptoms persist despite simple changes like staying hydrated and resting. Seek immediate attention if you experience vertigo or dizziness accompanied by chest pain, shortness of breath, severe headache, vision changes, difficulty speaking, weakness in your arms or legs, or confusion. These warning symptoms could indicate stroke, heart problems, or other serious conditions requiring urgent evaluation.
How Vertigo and Dizziness Are Diagnosed
Your doctor begins by asking detailed questions about your symptoms. When did they start? What exactly do you feel? What makes symptoms better or worse? Does moving your head in certain directions trigger vertigo? Do you have other health conditions or take medications? These questions help your doctor understand your specific situation.
Your doctor performs specific physical tests to identify the cause. For BPPV, the Dix-Hallpike test involves moving your head in specific ways while watching your eye movements. The Romberg test checks your balance. Your doctor performs a complete neurological examination, checking your strength, coordination, and other functions.
Your doctor may perform hearing tests to check if inner ear problems are present, vestibular testing to assess your balance system’s function, blood tests to rule out blood pressure problems, anemia, or infections, and sometimes MRI or CT scans to rule out brain-related causes. This comprehensive approach helps identify the exact source of your symptoms.
Treatment for Vertigo
The treatment for vertigo depends on its cause. For BPPV, the most common cause, treatment involves specific head positioning maneuvers performed by a therapist. The Epley maneuver is the most effective treatment for BPPV, working by repositioning the displaced crystals back to their proper location. Most people experience significant improvement after one to three sessions of these maneuvers.
Vestibular rehabilitation therapy teaches your brain to compensate for inner ear problems through specific exercises. Physical therapists guide you through movements that help your balance system adjust and recover. This therapy is remarkably effective and works by harnessing your brain’s ability to adapt and relearn balance. Over time, these exercises help your nervous system recalibrate and restore normal balance function.
Medications can help manage vertigo symptoms temporarily, including anti-nausea medications and medications that reduce dizziness. However, medication is usually temporary while you are receiving other treatments. The goal is to address the underlying cause rather than mask symptoms with medication alone.
Treatment for Dizziness
Treatment depends on the cause. If dehydration is causing dizziness, drinking water and maintaining hydration resolves it. If blood pressure is the issue, managing your blood pressure through lifestyle changes or medications helps. If a medication is causing dizziness, your doctor might adjust the dosage or switch to a different medication. If anemia is the cause, addressing the anemia through diet changes, supplements, or further investigation resolves the dizziness.
Treating underlying anxiety, managing stress through relaxation techniques, correcting vision problems, and addressing any medical conditions all help resolve dizziness. Once the root cause is treated, the dizziness typically disappears.
Understanding Syncope (Fainting)
Syncope, or fainting, is a temporary loss of consciousness due to reduced blood flow to the brain. Unlike other conditions, syncope involves actually losing consciousness, even if only briefly. Most people regain consciousness within seconds to minutes.
The most common type of syncope is vasovagal syncope, where your blood pressure suddenly drops in response to an emotional trigger like fear, pain, or sudden stress. Your heart rate may slow down, blood vessels relax, and blood pools in your legs, reducing blood flow to the brain. Other causes include problems with heart rhythm or structure, blood pressure problems, medications, and dehydration. Understanding which type you experience helps determine the right treatment.
Recognizing Signs of Syncope
Before fainting, people often experience warning signs. You might see spots or blurred vision, feel sudden lightheadedness, feel warm or flushed, experience nausea, feel weakness, and get a feeling that you are about to lose consciousness. These warning signs last seconds to a minute before fainting occurs. Importantly, not everyone gets warning signs, which is why some people faint suddenly without any notice.
During a fainting episode, you lose consciousness and may fall. You cannot respond to people around you. When regaining consciousness, you may feel confused, disoriented, or weak. Some people have little memory of the episode. The recovery period is usually brief, though you may feel shaky or tired afterward.
When Syncope Requires Urgent Care
If you faint once and are otherwise healthy, you may not need emergency care, but you should see a doctor to determine the cause. However, call emergency services immediately if fainting is accompanied by chest pain, irregular heartbeat, or shortness of breath, if you have a severe headache or remain confused after fainting, if you fainted while sitting or lying down, if you fainted more than once, if you did not have warning signs, if you took longer than a few minutes to regain consciousness, or if you have a known heart condition. These situations require urgent medical evaluation.
How Syncope Is Diagnosed
Your doctor asks detailed questions about what you were doing when you fainted, whether you had warning signs, and how quickly you regained consciousness. They perform a physical examination, check your heart rate and blood pressure, and perform blood tests to rule out anemia or blood sugar problems.
Depending on your situation, your doctor may order an ECG (heart tracing) to check your heart rhythm, a tilt table test where your body position is gradually changed while monitoring your heart and blood pressure, or sometimes an ultrasound of your heart. These tests help identify the cause of fainting and guide treatment decisions.
Living Well With Vertigo, Dizziness, or Syncope
Once you have been diagnosed and begin treatment, most people experience significant improvement. BPPV typically improves within a few weeks of repositioning maneuvers. Dizziness improves once its underlying cause is addressed. Syncope, once evaluated and managed, typically prevents future episodes.
For ongoing management, simple strategies help tremendously. Staying well hydrated by drinking water consistently, avoiding sudden position changes by standing up slowly, managing medications properly, reducing stress through relaxation techniques, treating any underlying medical conditions, and maintaining good balance through activities like tai chi or yoga all support recovery and prevent relapse. These lifestyle approaches complement medical treatment and promote long-term wellbeing.
Why You Should See a Neurologist
A neurologist specializes in nervous system disorders and is particularly helpful for vertigo and balance disorders. While your primary care doctor can address simple causes, a neurologist can evaluate complex cases, order specialized tests, manage ongoing vestibular problems, and coordinate comprehensive rehabilitation. They can distinguish between peripheral vertigo (from the inner ear) and central vertigo (from the brain), which require different management approaches.
You should see a neurologist if your vertigo or dizziness persists despite initial treatment, if you have recurrent episodes, if you also have other neurological symptoms, or if the cause remains unclear after initial evaluation. A neurologist’s expertise can be particularly valuable in complex cases where multiple conditions might be involved.
Frequently Asked Questions About Vertigo, Dizziness, and Syncope
What is the difference between BPPV and other types of vertigo?
BPPV is caused by misplaced crystals in your inner ear that respond to head movements. Other types of vertigo may result from infection, inflammation, or brain problems. BPPV is very treatable with specific repositioning maneuvers that move the crystals back into place.
How quickly does BPPV treatment work?
Many people experience relief within one to three sessions of the Epley maneuver. Some people notice improvement immediately after treatment. Most people become completely symptom-free within a few weeks.
Can vertigo or dizziness come back?
Yes, some conditions can recur. BPPV has a recurrence rate of about 15-50% over time. However, when it does recur, you know the diagnosis and treatment, making management straightforward and quick.
Will I always have this spinning sensation?
No. Most causes of vertigo are temporary and treatable. With proper treatment, the spinning sensation resolves. Even in cases requiring longer treatment, symptoms typically improve significantly.
Why did I faint if I have no heart problems?
Fainting can occur for many reasons unrelated to heart problems, including emotional reactions, dehydration, sudden blood pressure drop, or low blood sugar. Your doctor can determine the specific cause through evaluation.
Is it dangerous to faint?
Most fainting is not dangerous itself, though you could be injured from falling. However, repeated unexplained fainting or fainting with warning signs like chest pain requires medical evaluation to rule out serious conditions.
Can stress cause vertigo?
Stress and anxiety can cause dizziness and may trigger vertigo in susceptible people. Managing stress through relaxation techniques, exercise, meditation, or counselling helps reduce stress-related symptoms significantly.
What can I do to prevent vertigo or dizziness?
Stay well hydrated, move slowly when changing position, manage stress, take medications as prescribed, maintain good nutrition, treat underlying health conditions, and get adequate sleep. These simple measures prevent many cases of vertigo and dizziness.
How long does vestibular rehabilitation take?
Most people work with a physical therapist for several weeks, typically with 2-3 sessions per week. Many experience improvement within 2-4 weeks, though some people benefit from longer treatment as their brain continues to adapt.
Can I drive if I have vertigo?
During active vertigo, driving is not safe. Once your vertigo improves with treatment and you no longer have sudden episodes, your doctor can clear you to drive safely.
Should I stay in bed when I have vertigo?
Movement actually helps with vertigo recovery, especially when doing prescribed vestibular rehabilitation exercises. Bed rest may prolong recovery. Work with your therapist on appropriate movement and graduated activity.
Important Note
This page is for educational purposes only. It cannot replace a personal consultation with a doctor who knows your full medical history. If you are experiencing new or persistent vertigo, dizziness, or syncope, seek medical advice promptly.
This content does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for questions about your health.
Last Updated: November 2025
More Information & Next Steps
If you are looking for more information or want to discuss your symptoms with a specialist, you can use the links below:
